0353
Motion-corrected multi-shot EPI: Viable alternative to GRE for blood sensitive imaging with improved image quality and reduced scan time
Zhiqiang Li1, James Murchison1, Dori Shoshan1, Melvyn B Ooi2, and John P Karis1
1Barrow Neurological Institute, Phoenix, AZ, United States, 2Philips Healthcare, Houston, TX, United States
1Barrow Neurological Institute, Phoenix, AZ, United States, 2Philips Healthcare, Houston, TX, United States
Synopsis
Keywords: Motion Correction, Motion Correction, artifact, rapid scan, clinical study, high value
A motion-corrected 2D multi-shot EPI (msEPI) technique was compared to conventional 2D GRE to determine if it can be used as a faster technique for blood sensitive imaging in the emergency department (ED) setting. msEPI was found to be superior to GRE (p < 0.001) in motion artifact, overall image quality, and lesion detection. These results and reduced scan time make the motion-corrected 2D msEPI a viable alternative for blood sensitive imaging in the ED setting.Introduction
In the emergency department (ED) setting, brain MRI requires highly time efficient acquisition protocols in order to provide timely patient care as well as maintain patient throughput 1. A critical component of ED brain MRI is a T2* sensitive series that detects pathologic hemorrhage. T2* GRE is generally favored over susceptibility-weighted imaging (SWI) as a more time efficient technique. The standard of care GRE sequence at our institution contributes to approximately 30% of the total exam time (approximately 2 minutes of an 8-minute examination). We previously attempted to implement a T2* sequence utilizing multi-shot EPI (msEPI) technique that allows for more rapid image acquisition; however, this imaging technique often suffered from patient motion-induced artifacts. Several motion correction techniques have been developed for msEPI-based DWI that have demonstrated the ability to reduce both motion and phase errors 2-5. In this study we evaluated a novel new sequence, motion-corrected msEPI 6, to determine if it can be used as an even faster technique for blood sensitive imaging in the ED setting.Methods
Patient Population:This prospective study was performed at a single clinical site and was approved by the institutional review board. Emergency department patients undergoing non-emergent stroke imaging were eligible for inclusion. A total of 137 subjects were imaged (57 males, 80 females, 50.9 mean age, 9-90 age range) and analyzed.
Imaging Methods:
The study was performed on a single 1.5T MR scanners (Phillips Healthcare). The imaging parameters of standard of care GRE sequence as well as the motion-corrected msEPI 6 are listed in Table 1.
Radiologic Assessment:
Two radiologists performed review of all 137 subjects, and consensus scoring was obtained. For each subject, the matching pair of GRE and motion-corrected msEPI was compared side-by-side and scored relative to one another on four metrics: motion artifact, skull base susceptibility artifact, overall image quality, and lesion conspicuity (marked NA if no lesion visible). Each metric was scored on an ordinal 5-point Likert scale: 1 = GRE much better; 2 = GRE better; 3 = Comparable; 4 = msEPI better; 5 = msEPI much better. GRE and msEPI scans were randomized (left versus right) and anonymized for review. Additional sequences were made available at request of the radiologist to confirm presence of lesion. Susceptibility artifact associated with adjustable shunt valves and postoperative pneumocephalus were also included in evaluation of skull base susceptibility artifact as they degrade image quality. T2-bright lesions (arachnoid cysts, cystic encephalomalacia without hemosiderin staining, etc.) and those originating from the skull base were not considered for scoring of lesion conspicuity as these lesions do not show susceptibility and thus were not considered a T2* imaging lesion.
Statistical Analysis:
Nonparametric statistics were used due to ordinal scoring data. One-sample Wilcoxon signed rank test was used to compare GRE versus motion-corrected msEPI. We tested the null hypothesis H0: Δ = 3 versus H1: Δ ≠ 3 where Δ is the average of the two scores over the subject population for a given metric since a score 3 means msEPI is comparable with GRE. Rejection of the null hypothesis H1 suggests that the scoring distribution is not symmetric about 3 but in favor of either GRE Δ < 3 or msEPI Δ > 3. A p value of < 0.05 was chosen for statistical significance (H1).
Results and Discussion
The reading scores are shown in Fig. 1. For motion artifact, motion-corrected msEPI was superior to GRE (p < 0.001, Fig. 1a). Some representative examples are shown in Fig. 2. When significant motion artifact was present, some GRE images were nondiagnostic in comparison to the motion-corrected msEPI images, and may be repeated by the technician according to protocol (Fig. 2, last column). This repeated exam resulted in longer overall exam times. Only three subjects had worse motion artifact associated with msEPI compared to GRE, which may be attributed to randomly increased patient motion during msEPI acquisition compared to GRE.Motion-corrected msEPI demonstrated better overall image quality when compared with GRE (p < 0.001, Fig. 1b). Both reviewers noted that although overall signal was decreased with msEPI compared to GRE, contrast resolution and sharpness were improved and both reviewers preferred the appearance of msEPI images compared with GRE.
Motion-corrected msEPI was also superior to GRE for lesion detection (p < 0.001, Fig. 1c), as demonstrated in Fig 3. Every lesion identified on GRE was also identified on msEPI, but some lesions, particularly tubular lesions such as developmental venous anomalies were only identified on msEPI (Fig. 3, case 3).
Fig. 4 illustrates two examples of susceptibility-induced artifacts. GRE was superior to msEPI for skull base susceptibility artifact (p < 0.001, Fig. 1d) as expected because msEPI was designed to have increased susceptibility-induced signal loss due to longer effective TE. This also served as an internal control to ensure appropriate T2* weighting of msEPI images. Note that increased skull base susceptibility artifact did not negatively impact image quality or lesion detection.
Conclusion
Improved image quality and reduced scan time achieved by replacing GRE with motion corrected ms-EPI makes this new technique a viable alternative for blood sensitive imaging in the ED setting.Acknowledgements
The authors thank Dr. Guruprasad Krishnamoorthy and Philips Healthcare for their research support.References
- Sánchez Y, Yun BJ, Prabhakar AM, et al. Magnetic Resonance Imaging Utilization in an Emergency Department Observation Unit. West J Emerg Med. 2017;18:780-784.
- Porter DA, Heidemann RM. High resolution diffusion-weighted imaging using readout-segmented echo-planar imaging, parallel imaging and a two-dimensional navigator-based reacquisition. Magn Reson Med. 2009;62:468–475.
- Jeong H-K, Gore JC, Anderson AW. High-resolution human diffusion tensor imaging using 2-D navigated multishot SENSE EPI at 7 T. Magn Reson Med. 2013;69:793-802.
- Guhaniyogi S, Chu M-L, Chang H-C, Song AW, Chen N-K. Motion immune diffusion imaging using augmented MUSE for high-resolution multi-shot EPI. Magn Reson Med. 2016;75:639-652.
- Steinhoff M, Mertins A, Bornert P. SENSE-based multi-shot DWI reconstruction with extra-navigated rigid motion and contrast correction for brain EPI. In Proceeding of the ISMRM & SMRT Virtual Conference. 2020:4339.
- Li Z, Ooi MB, Karis JP. A rapid motion-corrected T2*-weighted multi-shot EPI technique for the Emergency Department setting. In Proceeding of the SMRM-ESMRMB Joint Annual Meeting. 2022:0756.
Figures
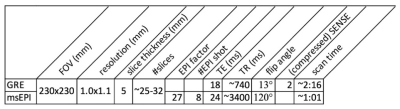
Table 1 Imaging parameters of standard of care GRE and the proposed msEPI.
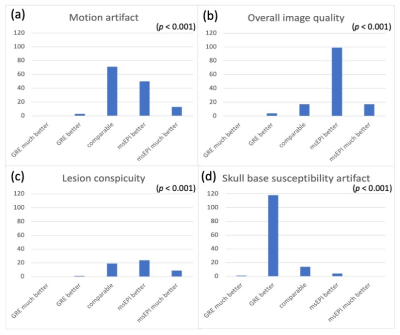
Fig. 1 Reading scores for GRE and msEPI in motion artifacts, overall image quality, lesion conspicuity, and skull base susceptibility artifact. Only cases with T2* imaging lesions were included for scoring of lesion conspicuity, while cases with T2-bright lesions and lesions originating from the skull base were not considered T2* imaging lesion and excluded.
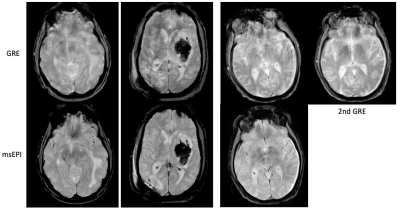
Fig. 2 Comparison of motion artifacts between GRE (top) and msEPI (bottom) in 3 patients. In case 3, the tech rescanned GRE after msEPI but the second GRE (last column) still suffered from moderate motion artifacts.
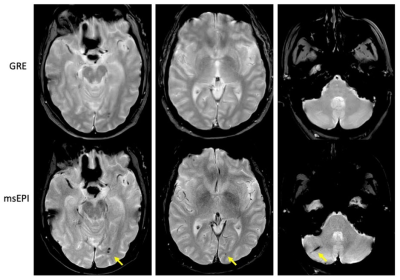
Fig. 3 Comparison of lesion conspicuity between GRE (top) and msEPI (bottom) in 3 patients. The lesions pointed to by the yellow arrows are better visualized in msEPI images. The developmental venous anomaly shown in case 3 is only identified in msEPI.
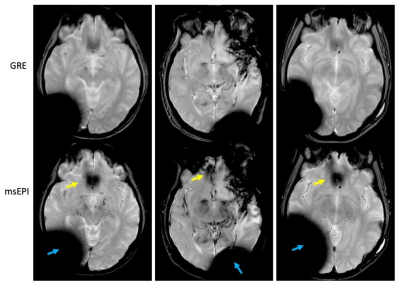
Fig. 4 Comparison of susceptibility artifacts between GRE (top) and msEPI (bottom) in 3 patients. msEPI shows slightly increased susceptibility induced signal loss in the frontal lobe (yellow arrows) and near metals (blue arrows).
DOI: https://doi.org/10.58530/2023/0353