0343
Diagnostic pearls and potential pitfalls of free-breathing motion-corrected LGE: a prospective head-to-head comparative study1Department of Radiology, Xiangya Hospital Central South University, Changsha, China, 2Scientific Marketing, Siemens Healthineers Ltd., Wuhan, China, 3MR Collabration, Siemens Healthineers, Los Angeles, CA, United States
Synopsis
Keywords: Cardiomyopathy, Myocardium, Late gadolinium enhancement
This study investigated the advantages and potential disadvantages of the MOCO-LGE sequence. The results showed that MOCO-LGE can effectively improve the image quality compared to BH-LGE. Meanwhile, the MOCO-LGE images could overestimate epicardial hyperenhancement and pericardial effusion, which might lead to overdiagnosis of myocarditis in clinical work. The study indicates that further refinement of this useful sequence may be needed.Introduction
Free-breathing motion-corrected (MOCO) late-gadolinium-enhancement (LGE) have been developed and approved for clinical use [1-4]. It is important to understand the overall advantages and disadvantages of MOCO-LGE to correctly interpret the results in clinic. The purpose of this prospective intraindividual study was to conduct a quantitative head-to-head comparison of MOCO-LGE and breath-held LGE (BH-LGE) in patients with cardiac disease.Method
Fifty consecutive patients with cardiac disease underwent MOCO-LGE and BH-LGE sequences [5] in random order on a 3T MR system (Prisma, Siemens Healthcare, Germany). Semi-quantitative image quality (IQ) scores, contrast-to-noise ratios (CNRs), quantitative size of myocardial scar and thickness of pericardial effusion were evaluated on short-axis phase-sensitive inversion recovery (PSIR) images of MOCO-LGE and BH-LGE.Result
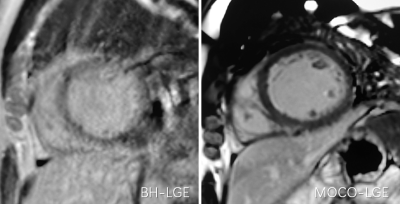
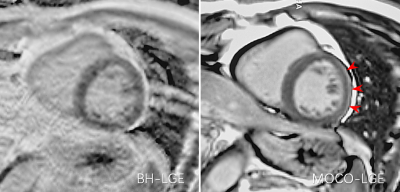
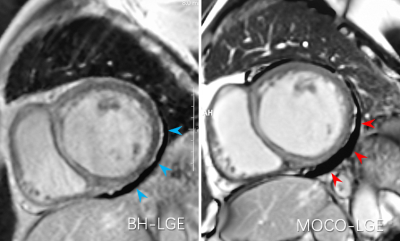
The MOCO-LGE images had better IQ scores than the BH-LGE images (4.12 ± 0.66 vs. 3.56 ± 0.81, p < 0.001) (Figure 1). The MOCO-LGE images showed higher CNR of the scar to the left ventricle (LV) cavity (21.77 ± 21.96 vs. 8.37 ± 9.03, p < 0.001) and the LV cavity to the remote myocardium (31.21 ± 20.00 vs. 19.02 ± 11.51, p < 0.001) than the BH-LGE images, but the difference of the CNR of the scar to the remote myocardium between the two images was not significant (9.88 ± 11.68 vs. 8.91 ± 9.99, p = 0.405). More epicardial hyperenhancement were seen in MOCO-LGE than BH-LGE (78% vs. 40%, p = 0.002) (Figure 2) and scar size measured by MOCO-LGE was more than BH-LGE (12.70 ± 12.25% vs. 7.15 ± 7.72%, p = 0.002) using 5-standard deviation method. More and thicker epicardial effusion were seen in MOCO-LGE than BH-LGE (86% vs. 60%, p = 0.001 and 7.04 ± 4.73mm vs. 3.77 ± 4.18mm, p < 0.001) (Figure 3).Discussion
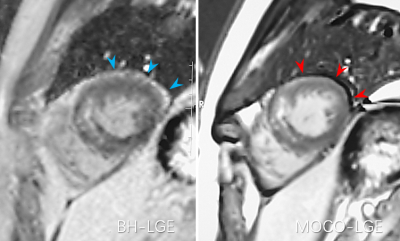
This was a preliminary prospective intraindividual head-to-head comparative study of MOCO-LGE with BH-LGE for the comprehensive evaluation of MOCO-LGE. The results suggest that the IQ scores and CNRs of MOCO-LGE can be improved, which was similar to previous several studies [1-4]. Moreover, the current study differs from prior studies in that we found the possible disadvantages of this sequence. Overestimation of epicardial hyperenhancement and pericardial effusion may lead to overdiagnosis of myocarditis in clinic. This potential disadvantage may be caused by the partial volume effects due to epicardial fat and water [6]. We also found that a portion of epicardial fat was shown as black in MOCO-PSIR-LGE images (Figure 4), which may help explain why the pericardial effusion appeared thicker on the MOCO-LGE images.Conclusion
MOCO-LGE may provide better image quality than BH-LGE, however MOCO-LGE may has the potential to overestimate the extent of epicardial hyperenhancement and pericardial effusion.Acknowledgements
This work was supported by Natural Science Foundation ofHunan Province, China (2021JJ31131).References
1 Cha MJ, Cho I, Hong J, et al. Free-Breathing Motion-Corrected Single-Shot Phase-Sensitive Inversion Recovery Late-Gadolinium-Enhancement Imaging: A Prospective Study of Image Quality in Patients with Hypertrophic Cardiomyopathy. Korean J Radiol. 2021;22(7):1044-1053. doi:10.3348/kjr.2020.1296
2 Captur G, Lobascio I, Ye Y, et al. Motion-corrected free-breathing LGE delivers high quality imaging and reduces scan time by half: an independent validation study. Int J Cardiovasc Imaging. 2019;35(10):1893-1901. doi:10.1007/s10554-019-01620-x
3 Olivieri L, Cross R, O'Brien KJ, Xue H, Kellman P, Hansen MS. Free-breathing motion-corrected late-gadolinium-enhancement imaging improves image quality in children. Pediatr Radiol. 2016;46(7):983-990. doi:10.1007/s00247-016-3553-7
4 Xie LJ, Xu R, Xu ZY, et al. Myocardial motion-corrected phase-sensitive inversion recovery late gadolinium enhancement in free breathing paediatric patients: a comparison with single-shot coherent gradient echo ("TrueFISP") phase-sensitive inversion recovery. Clin Radiol. 2021;76(6):471.e17-471.e25. doi:10.1016/j.crad.2021.01.018
5 Yan C, Hu J, Li Y, et al. Motion-corrected free-breathing late gadolinium enhancement combined with a gadolinium contrast agent with a high relaxation rate: an optimized cardiovascular magnetic resonance examination protocol. J Int Med Res. 2020;48(10):300060520964664. doi:10.1177/0300060520964664
6 Krupa K, Bekiesińska-Figatowska M. Artifacts in magnetic resonance imaging. Pol J Radiol. 2015 Feb 23;80:93-106. doi: 10.12659/PJR.892628. PMID: 25745524; PMCID: PMC4340093.
Figures