0325
18F-PSMA-1007 PET/MR compared to PET/CT in prostate cancer recurrence: impact on clinical management
1Derpartment of Circulation and Medical Imaging, Norwegian University of Science and Technology, Trondheim, Norway, 2PET Imaging Centre, University Hospital of North Norway, Tromsø, Norway, 3PET-Centre, Aarhus University Hospital, Aarhus, Denmark, 4Department of nuclear medicine, Oslo University Hospital, Oslo, Norway, 5The Cancer Clinic, St. Olavs Hospital, Trondheim, Norway, 6Department of Clinical and Molecular Medicine, Norwegian University of Science and Technology, Trondheim, Norway, 7Department of Radiology and Nuclear Medicine, St. Olavs Hospital, Trondheim, Norway
Synopsis
Keywords: Prostate, PET/MR
For patients with suspected prostate cancer recurrence, we examined the added value of 18F-PSMA-1007 PET to MR and CT imaging, and whether choice of PET modality, i.e. PET/MR or PET/CT, had an impact on clinical management. An intention-to-treat analysis was performed using findings from MR and CT alone, MR and CT with PET from PET/CT, and MR and CT with PET from PET/MR. Addition of 18F-PSMA PET changed clinical management in over 40% of patients. Differences in clinical management between PET/CT and PET/MR were smaller than adding any PET modality to MR and CT.
Introduction
Prostate-specific membrane antigen (PSMA) positron emission tomography (PET) imaging has been shown to impact clinical management for biochemical recurrence in prostate cancer (BCR)1–5. In select centers, PET/MR is an option to the more commonly available PET/CT. Recent studies comparing 68Ga-PSMA-11 PET/MR and 68Ga-PSMA-11 PET/CT have found that the detection rate of PET/MR is at least as high as PET/CT for detection of lymph node and distant metastases6,7, and superior for detecting local recurrences8. 18F-PSMA-1007 is an alternative tracer to 68Ga-PSMA-11, with potentially more favorable characteristics for detecting local recurrences because of minimal urinary excretion9,10.In this work, a head-to-head comparison of 18F-PSMA-1007 PET/MR and 18F-PSMA-1007 PET/CT was performed. The aim was to investigate the added value of PET to MR and CT imaging, and whether the choice of PET modality, i.e. PET/MR or PET/CT, has an impact on the clinical management for patients with BCR.
Methods
Retrospective data from 42 patients that had same-day 18F-PSMA-1007 PET/MR and PET/CT examinations due to BCR, were studied. The images were acquired at St. Olavs Hospital, Trondheim University Hospital, Norway. The study was approved by the regional ethical committee (REK 2019/238). Patient characteristics are summarized in Table 1. The imaging studies were randomly split into two datasets where each dataset contained PET from PET/MR for half of the patients (n = 21) and PET from PET/CT for the remaining image datasets (n = 21).The images were read by two independent sets of experienced readers from three institutions, each consisting of a radiologist and a nuclear medicine physician. With each reading, lesions were reported and scored using a five-point scale from benign to malignant, and an overall conclusion for the patient was reported. Each dataset was read at least two weeks apart. The reading of each dataset was performed as follows: The nuclear medicine physicians performed a reading based on the PET data using CT as an anatomical correlate. For the PET from PET/MR, a co-registered CT from the PET/CT was used. The radiologists read MR and CT data. A consensus reading between radiologist and nuclear medicine physician was performed where PET data from one modality and MR and CT data was available. Since there were no differences in data between the datasets in the radiologist readings, only a single dataset was read, and its findings were used in the consensus reading for both datasets.
Relevant clinical variables, medical history, reported imaging findings and overall reading conclusions were presented to a urologic oncologist to perform an intention-to-treat analysis. This analysis was performed for each set of reported readings using the two radiologist readings, and the four consensus readings, resulting in six intended treatment plans per patient. Each intention-to-treat analysis was performed at least one week apart. An overview of the study design is presented in Figure 1.
In the intention-to-treat analysis, the following six treatment categories were used: androgen deprivation therapy (ADT) with confirmed metastatic disease (ADT M1), ADT without confirmed metastatic disease (ADT M0), salvage radiotherapy with ADT, treatment for oligometastatic disease, further examinations, and observation only. For non-systemic treatments or further examinations, it was verified that treatments were indeed the same by targeting the same lesion or suggesting the same follow-up examinations.
Results
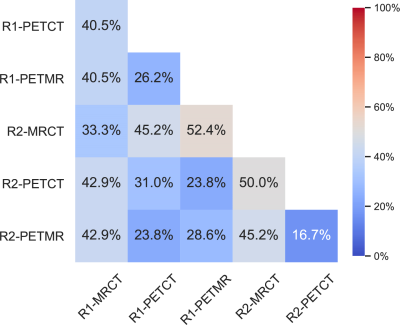
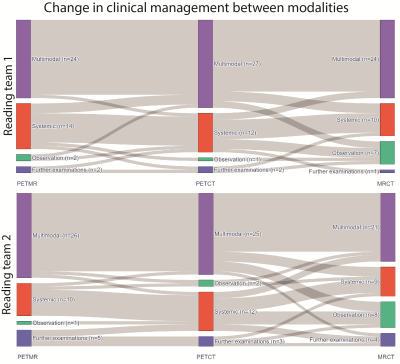
A change in clinical management between reading teams for the same modality was found in 12 patients (29%) in consensus reading with PET from PET/MR, 13 patients (31%) in consensus reading with PET from PET/CT and 14 (33%) in the radiologist readings.Between modalities for the same readers, a difference in intended clinical management was found in 7 patients (17%) and 11 patients (26%) between consensus readings with PET from PET/MR and PET from PET/CT for each of the reading teams respectively. Between radiologist readings and consensus readings, a change in clinical management was observed in between 17 patients (40%) and 21 patients (50%), respectively. An overview of the observed changes in clinical management between datasets is shown in Figure 2.
Figure 3 shows change in treatment category between modalities. Without PSMA PET, a larger number of patients end up with observation only.
Discussion
We found 18F-PSMA-1007 PET to change the intended clinical management in over 40% of patients when compared to using MR and CT imaging only. This result is in line with recent reviews that report an overall change in clinical management of 56.4%11 and a major change in clinical management in 42.7%12 after PSMA PET in patients with BCR.When comparing the same modality between readers, we found a considerable discrepancy in intended clinical management. This discrepancy can not only be attributed to differences in readers interpretation, but also reflect the intrareader variability in the urologic oncologist’s opinion presented with similar findings.
Conclusion
18F-PSMA-1007 PET changed the intended clinical management in over 40% of patients compared to using MR and CT imaging only. The impact of adding PET is larger than the differences found between PET/MRI and PET/CT.Acknowledgements
No acknowledgement found.References
1. Roach, P. J. et al. The Impact of 68Ga-PSMA PET/CT on Management Intent in Prostate Cancer: Results of an Australian Prospective Multicenter Study. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 59, 82–88 (2018).
2. Farolfi, A. et al. 68Ga-PSMA-11 PET/CT in prostate cancer patients with biochemical recurrence after radical prostatectomy and PSA <0.5 ng/ml. Efficacy and impact on treatment strategy. Eur. J. Nucl. Med. Mol. Imaging 46, 11–19 (2019).
3. Afaq, A. et al. Impact of 68Ga-Prostate-Specific Membrane Antigen PET/CT on Prostate Cancer Management. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 59, 89–92 (2018).
4. Calais, J. et al. Impact of 68Ga-PSMA-11 PET/CT on the Management of Prostate Cancer Patients with Biochemical Recurrence. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 59, 434–441 (2018).
5. Bashir, U. et al. Impact of Ga-68-PSMA PET/CT on management in prostate cancer patients with very early biochemical recurrence after radical prostatectomy. Eur. J. Nucl. Med. Mol. Imaging 46, 901–907 (2019).
6. Freitag, M. T. et al. Comparison of hybrid 68Ga-PSMA PET/MRI and 68Ga-PSMA PET/CT in the evaluation of lymph node and bone metastases of prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 43, 70–83 (2016).
7. Jentjens, S. et al. Prospective comparison of simultaneous [68Ga]Ga-PSMA-11 PET/MR versus PET/CT in patients with biochemically recurrent prostate cancer. Eur. Radiol. 32, 901–911 (2022).
8. Guberina, N. et al. Whole-Body Integrated [68Ga]PSMA-11-PET/MR Imaging in Patients with Recurrent Prostate Cancer: Comparison with Whole-Body PET/CT as the Standard of Reference. Mol. Imaging Biol. (2019) doi:10.1007/s11307-019-01424-4.
9. Giesel, F. L. et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur. J. Nucl. Med. Mol. Imaging 44, 678–688 (2017).
10. Arnfield, E. G. et al. Clinical insignificance of [18F]PSMA-1007 avid non-specific bone lesions: a retrospective evaluation. Eur. J. Nucl. Med. Mol. Imaging 48, 4495–4507 (2021).
11. Pozdnyakov, A. et al. The impact of PSMA PET on the treatment and outcomes of men with biochemical recurrence of prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 1–9 (2022) doi:10.1038/s41391-022-00544-3.
12. Mazrani, W., Cook, G. J. R. & Bomanji, J. Role of 68Ga and 18F PSMA PET/CT and PET/MRI in biochemical recurrence of prostate cancer: a systematic review of prospective studies. Nucl. Med. Commun. 43, 631–637 (2022).
Figures
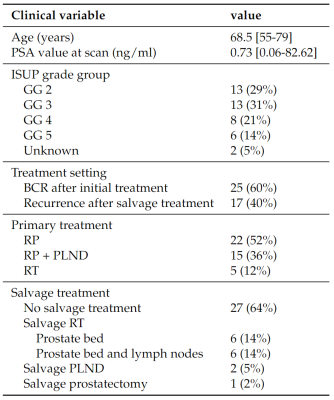
Table 1 Patient characteristics. PSA = Prostate-specific membrane antigen, ISUP = The International Society of Urological Pathology, GG = grade group, BCR = biochemical recurrence, RP = radical prostatectomy, PLND = pelvic lymph node dissection, RT = radiotherapy.
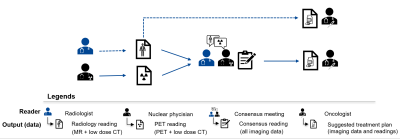
Figure 1 Study design. PET and CT images were read by nuclear medicine physicians. MR and CT images were read by radiologists. A consensus reading was performed between radiologist and nuclear medicine physician using all available image data. Nuclear medicine physician readings and consensus readings were performed for datasets containing half PET from PET/MR and half from PET/CT. Consensus readings and radiologist readings were used in an intention-to-treat analysis performed by a urologic oncologist.