0315
Assessment of Background Heterogeneity of Prostate Peripheral Zone for Cancer Detectability using Magnetic Resonance Fingerprinting
Peter Qiao1, Donald Brennan1, Sree Harsha Tirumani2,3, Yong Chen2,3, Mark Griswold2,3, and Leonardo Kayat Bittencourt2,3
1School of Medicine, Case Western Reserve University, Cleveland, OH, United States, 2Department of Radiology, Case Western Reserve University, Cleveland, OH, United States, 3Department of Radiology, University Hospitals Cleveland Medical Center, Cleveland, OH, United States
1School of Medicine, Case Western Reserve University, Cleveland, OH, United States, 2Department of Radiology, Case Western Reserve University, Cleveland, OH, United States, 3Department of Radiology, University Hospitals Cleveland Medical Center, Cleveland, OH, United States
Synopsis
Keywords: Prostate, Cancer
In this pilot study, we assessed the background signal change (BSC) of the prostate peripheral zone based on quantitative T1 and T2 measurement obtained using Magnetic Resonance Fingerprinting (MRF) and correlated with a previously-developed qualitative BSC score. Our results demonstrate the importance of prostate BSC toward reducing uncertainty in prostate MRI. Compared to the qualitative BSC score, the MRF-derived measurements provide a more reproducible and objective assessment of background heterogeneity of the prostate. BSC scoring has great potential in risk-stratifying patients with incidentally-detected clinically significant prostate cancer and yielding better biopsy decision-making for patients with negative MRI.Introduction
Prostate cancer is projected to be the most common form of cancer and second largest contributor to cancer-associated mortality in men (1). Present clinical strategies employ inadequate biopsy approaches leading to both under-diagnosis of clinically significant prostate cancer (csPCa) and over-diagnosis of insignificant prostate cancer. To better detect and guide biopsies, MRI has emerged as an informative, accompanying tool along with the Prostate Imaging Reporting and Data System (PI-RADS) for characterizing the risk of csPCa in focal lesions. However, the diagnosis and recognition of csPCa through MRI still has a notoriously steep learning curve. One of the major difficulties originates from the universally heterogeneous appearance of the peripheral zone of the gland, which houses 70% of detected prostate cancer. The varying degrees of T2-hypointense background signal changes (BSC) are the results of many influences, which can appear altogether as patchy areas of low signal intensity on standard T2-weighted images and mimic tumors or obfuscate true lesions that would otherwise be detected. Qualitative and semi-quantitative scoring systems have recently been proposed for indirect assessment of BSC in prostate peripheral zone. However, these approaches mostly rely on qualitative, subjective imaging features and are therefore limited with poor reproducibility and demonstrated difficulty in standardization (2). Magnetic Resonance Fingerprinting (MRF) technique is a new quantitative MR imagine technique, which can simultaneously quantify T1 and T2 relaxation times for prostate with superior repeatability and reproducibility (3-5). The objective of this study is to correlate MRF T1 and T2 measurements to a previously described, qualitative BSC score to evaluate its utility for assessing the intra-subject diagnostic uncertainty of prostate cancer on MRI.Methods
A total of 122 patients who received imaging studies compliant with PI-RADS 2.1 guidelines and MRF at our institute were retrospectively identified (6, 7). Demographic and clinical data was obtained from the electronic medical record. For each patient, a FISP-MRF sequence was performed at multiple axial slices on a 3T MRI scanner. The imaging parameters included: matrix size, 400x400; FOV, 40x40 cm2; TR, 13~15 ms; flip angle, 5~75 degrees; slice thickness, 6 mm; scan time, 40 sec. Quantitative T1 and T2 maps were computed offline using a pre-calculated MRF dictionary and template matching.For each patient, MRF-derived T1 and T2 relaxation times were measured in three axial slices, located at the apex, base, and mid-prostate. Two ROIs were drawn per axial slice, resulting in a total of six measured T1 and T2 times for each subject to calculate mean T1 and T2 values (Fig 1). Any focal suspicious peripheral zone lesions were excluded from the ROIs (Fig 1) to ensure the assessment of the background peripheral zone only. The qualitative BSC score for peripheral zone was determined using the criteria described in the literature (2). Signal intensity and percentage of peripheral zone involvement across six sectors was assessed on standard T2-weighted images for this evaluation. Furthermore, PI-RADS 2.1 scores were assigned to any suspicious lesion by one radiologist with 13 years of experience. Here, PI-RADS 1&2 represent low risk for csPCa (negative MRI), PI-RADS 3 represents equivocal lesions, and PI-RADS 4&5 represent high risk lesions, that should be biopsied.
Further analysis was performed in a subgroup of the patients with a negative MRI (PI-RADS 1&2) that had available follow-up biopsy (n=40). Any MRI-invisible csPCa detected in these patients during biopsy was correlated to the qualitative BSC score and MRF-derived T1/T2 values.
Results
Fig 2 shows the distributions of qualitative BSC scores and MRF-derived mean T1 and T2 values of the peripheral zone for the patient cohort (n=122). Fig 3 shows the distribution of the PI-RADS score vs BSC score. Based on MRF measurements, both T1 and T2 relaxation times in the peripheral zone were statistically significantly correlated with the BSC scores (Fig 4). When analyzing the subgroup of MRI-negative patients (PI-RADS 1&2) with a follow-up biopsy, MRF outperformed the qualitative BSC score in identifying patients at a higher risk for MRI-invisible csPCa (Fig 5). Average T1<1800ms and T2<100ms of the peripheral zone were independently capable of almost fully separating the patients showing incidental csPCa on follow-up biopsies, compared to a 1.6:1 separation from qualitative BSC scores.Discussion and Conclusion
This study demonstrates the utility of quantitative MRF measurements of prostate T1 and T2 values as surrogates for the qualitative BSC score. Our results show that the BSC score is correlated with a higher detection rate of PI-RADS 3 findings, suggesting an effect of background heterogeneity of the peripheral zone in introducing diagnostic uncertainty to prostate MRI, and leading to poor differentiation between true positive and true negative findings. Moreover, prominent BSC in patients with a negative MRI was associated with a higher rate of MRI-invisible cancers missed, underscoring the importance of incorporating BSC assessment to the reading routine of prostate MRI. And most importantly, compared to a subjective qualitative BSC score, the robust quantitative MRF T1 and T2 values provide a more reproducible and objective assessment of background heterogeneity of prostate, thus allowing for development of streamlined automated assessment of BSC, and have great potential in separating patients at risk for MRI-invisible csPCa, and thus yielding better biopsy avoidance decisions for patients with a negative MRI.Acknowledgements
Our group receives research support from Siemens Healthineers.References
1. Siegel RL, et al. Cancer Statistics, 2021; 7-33.
2. Bura V, et al. Eur Radiol, 2021; 4908-4917.
3. Ma D, et al. Nature, 2013; 187-192.
4. Yu A, et al. Radiology, 2017; 729-738.
5. Lo W, et al. MRM, 2022; 1818-1827.
6. Barrett T, et al. Clin Radiol, 2015; 1165-1176.
7. Barrett T, et al. N Engl J Med, 2021: 908-920.
Figures
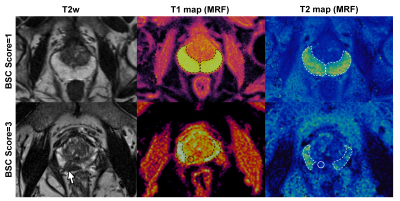
Figure 1. Representative
T2 weighted (T2w) images and T1 and T2 maps derived through MRF for low and
high BSC scores, with ROIs used for analysis illustrated. In the case with a
BSC score of 3, a hypointense
lesion (arrow) is noted and excluded from the ROI analysis.

Figure 2: (A)
Distribution of qualitative BSC scores in the patient cohort (n=122).
Distribution of MRF-derived mean T1 (B) and T2 (C) values of the peripheral
zone in the patient cohort.
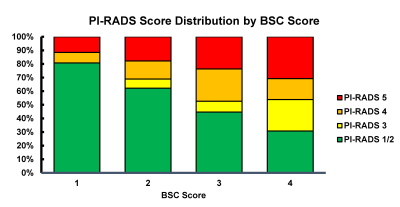
Figure 3: Distribution
of PI-RADS scoring vs qualitative BSC score. A greater percentage of equivocal
lesions (PI-RADS score, 3) were found in patients with greater peripheral
zone
heterogeneity and increasing BSC score. The percentage of detected PI-RADS 3
lesions increased with higher BSC scores, from 0% in BSC=1, up to 23% among
patients with BSC=4.
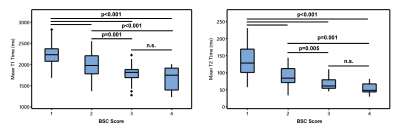
Figure 4: Mean
T1 and T2 relaxation times graphed by BSC score for prostate peripheral zone.
Patients with relatively homogenous peripheral zone (BSC score =1) demonstrated
significantly higher mean T1 and T2 times compared to those with heterogeneous
peripheral zone (BSC score =3, 4). n.s.=not
statistically significant.
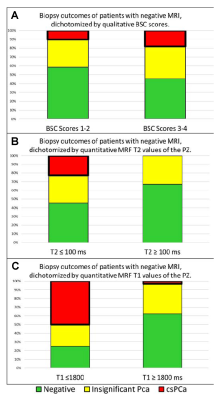
Figure
5.
MRF-derived T1 and T2 values of the peripheral
zone outperform qualitative BSC scores in identifying patients with csPCa
after a negative MRI (PI-RADS scores, 1 or 2). (A) Analysis based on the
qualitative BSC score. (B) Analysis based on a mean T2 threshold value of 100 ms. (C)
Analysis based on a mean T1 threshold value of 1800 ms.
DOI: https://doi.org/10.58530/2023/0315