0197
The performance of evaluation in neoadjuvant chemotherapy for breast cancer on abbreviated breast MRI: comparison with full diagnostic protocol1Guangzhou First People's Hospital, Guangzhou, China, 2Philips Healthcare, Guangzhou, China
Synopsis
Keywords: Breast, Cancer, Breast neoplasms, Neoadjuvant chemotherapy, Radiologists
To compare the diagnostic efficacy of abbreviated breast MRI (AB-MRI) and regular full diagnostic protocol MRI (FDP-MRI) in the assessment of response to neoadjuvant chemotherapy (NAC) in breast cancer, this study retrospectively analyzed the performance of AB-MRI and FDP-MRI in breast cancer patients undergoing NAC. We found that, for experienced radiologists, compared with FDP-MRI, AB-MRI showed similar sensitivity, specificity, and accuracy in the evaluation of pCR and similar accuracy in the measurement of residual tumor size for breast cancer.Introduction
Compared with the regular full diagnostic protocol MRI (FDP-MRI), abbreviated breast MRI (AB-MRI) reduces scan and interpretation times, it can potentially increase MRI accessibility while decreasing cost.1 In recent prospective studies with a large cohort, AB-MRI showed excellent performances in the screening of women with dense breasts or a history of breast cancer.2,3 A growing body of research showed that the diagnostic performances of AB-MRI are comparable to FDP-MRI in breast cancer screening.4,5 However, in most of the past studies, the study setting of AB-MRI was mostly in breast screening, while the studies on neoadjuvant chemotherapy (NAC) response evaluation were few. However, multiple MRI examinations are often required after NAC for breast cancer evaluation, which requires long image acquisition time, a high workload of radiologists, and affects the patient’s ability to tolerate these examinations alongside the cost of the examination. Thus, improving the availability and reducing the cost of MRI without compromising diagnostic performance is the key to the widespread application of MRI after NAC treatment. Therefore, the purpose of the study was to compare AB-MRI and FDP-MRI in performance for the evaluation of NAC in patients with breast cancer.Methods
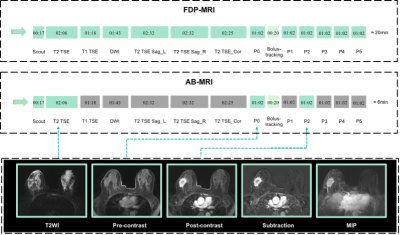
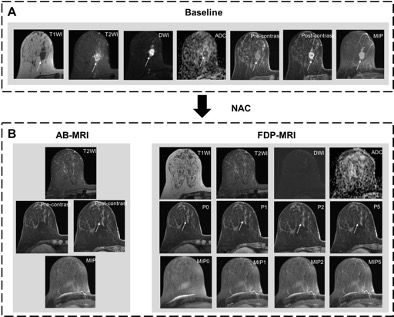
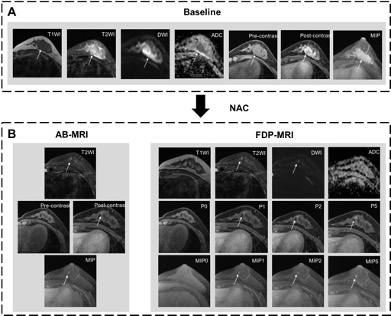
The patients with breast cancer who received NAC (all underwent MRI examination before NAC and after the last NAC) were retrospectively collected from two centers. Nine readers independently interpreted each AB-MRI and FDP-MRI. AB-MRI was extracted from FDP-MRI, including axial T2-weighted with fat saturation, axial T1-weighted images of pre- and early post-contrast phases, and their derived images (MIP images and subtraction images). (Figure 1). The diagnostic performance of AB-MRI and FDP-MRI was analyzed, including assessing pCR and residual tumor size, and the diagnostic efficacy was compared between readers. Diagnostic performance for determining pCR including sensitivity, specificity, and accuracy was calculated. Pearson’s correlation coefficients test was used to determine the association between the size of the residual tumor measured on AB-MRI or FDP-MRI and the pathologic size. Z-test was calculated to compare the correlation coefficient between MRI and pathological results.Results
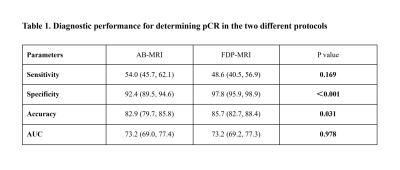
A total of 203 patients were enrolled in this study (mean age ± SD, 52.1 years±11.2; range, 27-88 years), of which 153 patients achieved non-pCR (75.4%) and 50 achieved pCR (24.6%). For overall performance, in the AB-MRI group, the sensitivity, specificity, accuracy, and AUC (composite indicator) were 54.0%, 92.4%, 82.9%, and 0.732, respectively; In the FDP-MRI group were 48.6%, 97.8%, 85.7% and 0.732, respectively (Table 2). The sensitivity of the AB-MRI group was comparable to that of the FDP-MRI groups (54.0% vs 48.6%, P=0.169). The specificity and accuracy of the AB-MRI group were lower than that of the FDP-MRI (specificity:92.4% vs 97.8%, P<0.001; accuracy: 82.9% vs 85.7%, P=0.031), which was mainly observed in the junior radiologists (P < 0.001 and =0.011, respectively). For experienced radiologists, there was no significant difference in sensitivity, specificity, accuracy or AUC between the AB-MRI and FDP-MRI groups (P > 0.05). The AUC was comparable in of AB-MRI and FDP-MRI groups (AUC: 0.732 vs 0.732, P=0.978) (Figure 2 and Figure 3, Table 1). For overall performance, the accuracy of AB-MRI and FDP-MRI measurements was not significantly different in evaluating residual tumor size (Z = -1.605, P = 0.109). But among the junior radiologists, the accuracy of FDP-MRI assessment was better than that of AB-MRI assessment (Z=-2.144, P=0.032).Discussion
Our dual-center, multi-reader study compared the performance of AB-MRI and FDP-MRI in the NAC evaluation of breast cancer. The two MRI protocols had similar sensitivity in assessing pCR, but AB-MRI had lower specificity and accuracy than FDP-MRI, which was mainly observed in junior radiologists. The rate of enhancement of residual cancer after NAC might be delayed because of the antiangiogenic effects of chemotherapy, resulting in misjudgment of AB-MRI.6,7 While, it may be overestimated on FDP-MRI due to reactive inflammation, fibrosis, or necrosis after NAC, which showed the enhanced area in the delayed phase.8,9 The two MRI protocols could reflect the size of the residual tumor well. The findings indicate the potential utility of AB-MRI in evaluating NAC response when radiologists had a certain experience.Conclusion
The AB-MRI does not affect the performance in the NAC response evaluation of breast cancer. This finding support implementation of AB-MRI in NAC response evaluation of breast cancer by experienced radiologists.Acknowledgements
No acknowledgment found.References
[1] Kuhl C, Schrading S, Strobel K, Schild H, Hilgers R, Bieling H (2014) Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 32:2304-2310
[2] Comstock C, Gatsonis C, Newstead G et al (2020) Comparison of Abbreviated Breast MRI vs Digital Breast Tomosynthesis for Breast Cancer Detection Among Women With Dense Breasts Undergoing Screening. JAMA 323:746-756
[3] Kim S, Cho N, Hong H et al (2022) Abbreviated Screening MRI for Women with a History of Breast Cancer: Comparison with Full-Protocol Breast MRI. Radiology. 10.1148/radiol.213310:213310
[4] Romeo V, Cuocolo R, Liuzzi R et al (2017) Preliminary Results of a Simplified Breast MRI Protocol to Characterize Breast Lesions: Comparison with a Full Diagnostic Protocol and a Review of the Current Literature. Academic radiology 24:1387-1394
[5] Al Ewaidat H, Ayasrah M (2022) A Concise Review on the Utilization of Abbreviated Protocol Breast MRI over Full Diagnostic Protocol in Breast Cancer Detection. International journal of biomedical imaging 2022:8705531
[6] Schrading S, Kuhl C (2015) Breast Cancer: Influence of Taxanes on Response Assessment with Dynamic Contrast-enhanced MR Imaging. Radiology 277:687-696
[7] Santamaría G, Bargalló X, Fernández P, Farrús B, Caparrós X, Velasco M (2017) Neoadjuvant Systemic Therapy in Breast Cancer: Association of Contrast-enhanced MR Imaging Findings, Diffusion-weighted Imaging Findings, and Tumor Subtype with Tumor Response. Radiology 283:663-672
[8] Yeh E, Slanetz P, Kopans D et al (2005) Prospective comparison of mammography, sonography, and MRI in patients undergoing neoadjuvant chemotherapy for palpable breast cancer. AJR American journal of roentgenology 184:868-877
[9] Reis J, Lindstrøm J, Boavida J et al (2020) Accuracy of breast MRI in patients receiving neoadjuvant endocrine therapy: comprehensive imaging analysis and correlation with clinical and pathological assessments. Breast cancer research and treatment 184:407-420
Figures