0186
A panoramic view for supine breast MRI1High Field MR Center, Center for Medical Physics and Biomedical Engineering, Medical University of Vienna, Vienna, Austria
Synopsis
Keywords: Breast, Visualization
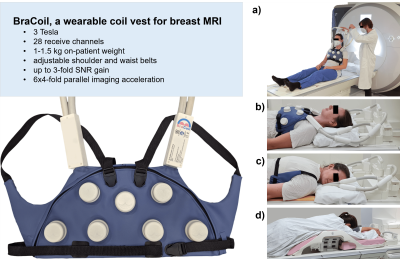
A wearable coil worn like a vest (“BraCoil”) has recently been shown to improve signal-to-noise ratio by a factor of up to three in supine breast MRI. However, the visualization of supine breast images is inefficient when using Cartesian views due to the bent shape of the breast along the chest wall. We introduce a panoramic view similar to panoramic dental X-ray to make reading of supine breast MRI more efficient by reducing the number of slices by a factor of 2-4, depending on breast size.Introduction
Breast cancer is the most common malignant cancer in women worldwide1. Screening programmes, typically using X-ray mammography, enable early detection and thereby reduce mortality. Breast MRI outperforms X-ray mammography in terms of sensitivity, in particular in women with dense breasts2,3, and does not involve ionizing radiation. A limitation of current breast MRI is the prone image acquisition, since the breast shape does not correlate well with other diagnostic and therapeutic procedures like ultrasound, biopsy, radiation therapy, and surgery, which are performed in the supine position. Therefore, supine MRI is a promising alternative, for which a dedicated wearable coil vest has been introduced4.Conventional breast MR images acquired in the prone position are usually displayed upside down in an axial Cartesian view. However, this view is not optimal for supine imaging because the breast tissue is flattened and is distributed over the chest wall. This reduces the axial cross-section of the breast considerably, which can make reading difficult. A coronal view may be suitable for supine imaging, but is still not optimal for viewing the lateral parts of the breast. In both cases (axial and coronal views), the reading time increases due to the large number of slices. Therefore, a new visualization paradigm for supine breast MR images is needed.
Methods
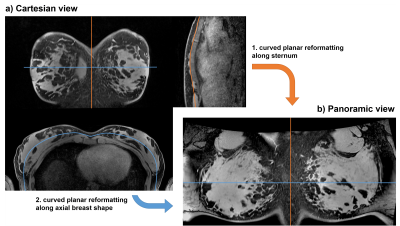
In vivo data were acquired from three healthy female volunteers (age 25-43) with small/medium-sized/large breasts (volumes 657/1338/3020mL) using a flexible wearable 28-channel Rx-only breast coil (BraCoil, Center for Medical Physics and Biomedical Engineering, Medical University of Vienna, Austria) in supine position on a 3T MR scanner (Prisma Fit, Siemens Healthineers, Erlangen, Germany). As a reference, a standard rigid breast coil (Breast 16 Sentinelle, Siemens Healthineers, Erlangen, Germany) was used in the prone position. Design features and positioning variants with the BraCoil in comparison to the clinical standard are shown in Fig. 1. Coronal T2-weighted turbo-spin echo images were obtained with the BraCoil, TR/TE=11540-16000/172 ms, in-plane resolution 0.5-0.6x0.5-0.6 mm², 64-88 slices with thickness 1.5-1.8 mm, turbo-factor 14, and acceleration factor 3-4. Axial T2-weighted turbo-spin echo images were acquired with the reference coil and the same imaging parameters except a slightly different range for TR=15300-15910 ms and the number of slices (85-88) to cover the whole breast. The study was approved by the Ethical Committee of the Medical University of Vienna (nr. 2137/2021) and informed written consent was obtained from all volunteers.Panoramas were created using 3D Slicer5,6 by applying two consecutive curved planar reformatting transforms7 along curves manually drawn on the T2-weighted images (Fig. 2). The first curve was drawn along the sternum in a central sagittal image. After the first flattening transform, the volume was rotated around the L-R axis to align the sternum in sagittal direction. The second curve followed the center of the breast tissue in an axial image through the fullest part of the breast.
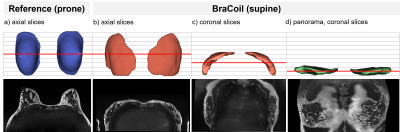
Breast tissue was manually segmented from isotropic (2.2 mm)³ 3D gradient-echo images acquired with the BraCoil in supine and the reference coil in prone position (Fig. 3a-c). The segmented volumes from supine acquisitions with the BraCoil were transformed in the panoramic view (Fig. 3d). All volumes were cropped to the extent of breast tissue (with >10 breast tissue voxels per slice), and the sizes of the volumes were determined to calculate the relative reduction in slices by applying the panoramic transform.
Results
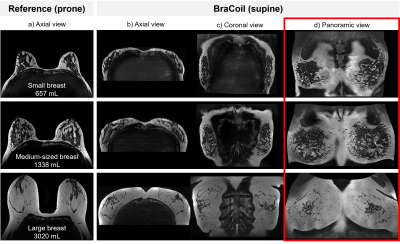
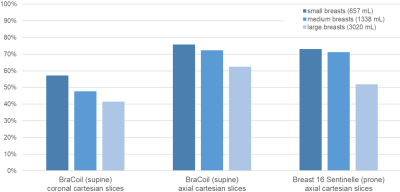
A comparison of axial, coronal, and panoramic views is shown in Fig. 4, demonstrating its benefit for all investigated breast sizes.Quantitatively, the panoramic view resulted in considerably fewer slices containing breast tissue. As presented in Fig. 5, compared to the reference, slice numbers were reduced by 52-73%. Similar results (62-76%) were obtained for the comparison to supine axial images. Against supine coronal data, the reduction was 42-57%. The advantage is consistently higher for smaller breast volumes than for larger breasts.
Discussion
In its current implementation, the technique still requires manual interaction for drawing two curves across the breast and along the sternum. Future development should aim at automatization of this process. Also, since the flattening of the breast is based only on these two lines, the flattening algorithm becomes less accurate towards the corners of the panoramic image. This shortcoming could be addressed by reformatting the images along a 3D-curved manifold following the shape of the chest wall8.The panoramic transformation leads to location-dependent geometric distortion and inhomogeneous spatial resolution across the image. However, the view is primarily intended to enable efficient reading and detection of lesions. Quantitative measurements, e.g. of lesion size, can be obtained by switching back to the original Cartesian view.
To determine the practical utility of the panoramic view and its performance in a clinical setting, further studies on patients with diagnostic work-up by experienced breast radiologists are currently being conducted.
Conclusion
We propose a panoramic visualization of breast images similar to dental panoramic X-ray, overcoming the limitations of the Cartesian view in supine breast MRI. It was shown to reduce the number of slices to be read by the radiologist by a factor of 2-4, depending on breast size.Acknowledgements
This work was funded by the joint Austrian/French grant “BRACOIL“ (Austrian Science Fund FWF Nr. I-3618/Agence Nationale de Recherche ANR-17-CE19-0022), the Austrian Society of Senology, and the Oesterreichische Nationalbank (Austrian Central Bank, Anniversary Fund, project nr. 17980 “FlexShim“).References
1. Kuhl, C. K. Underdiagnosis is the main challenge in breast cancer screening. The Lancet Oncology 20 1044–1046 (2019).
2. Mann, R. M. et al. Breast cancer screening in women with extremely dense breasts recommendations of the European Society of Breast Imaging (EUSOBI). Eur. Radiol. (2022) doi:10.1007/s00330-022-08617-6.
3. Sardanelli, F. et al. Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. Eur. J. Cancer 46, 1296–1316 (2010).
4. Obermann, M. et al. BraCoil – a wearable one-size-fits-all breast coil for 3 T MR mammography. in Proc. Intl. Soc. Mag. Reson. Med. 30 (2022) p.188.
5. Fedorov, A. et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 30, 1323–1341 (2012).
6. 3D Slicer image computing platform. 3D Slicer https://www.slicer.org/. [accessed 2022-11-09]
7. PerkLab/SlicerSandbox. GitHub https://github.com/PerkLab/SlicerSandbox/tree/master/CurvedPlanarReformat. [accessed 2022-11-09]
8. Kretschmer, J. et al. ADR--Anatomy-Driven Reformation. IEEE Trans. Vis. Comput. Graph. 20, 2496–2505 (2014).
Figures