0185
Personalized Breast MRI Scanning Using Deep Learning
Sarah Eskreis-Winkler1, Arka Bhowmik1, Christopher Comstock1, Elizabeth Sutton1, Vardan Sevilimedu1, Sunitha Thakur1, and Katja Pinker1
1MSK, New York, NY, United States
1MSK, New York, NY, United States
Synopsis
Keywords: Breast, Breast, Artificial Intelligence
Contrast-enhanced breast MRI exams typically last more than 20 minutes even though the dynamic contrast-enhanced sequences alone would be sufficient for interpretation in over 95% of cases. Thus, we present a personalized on-the-fly MRI protocoling paradigm, where a deep learning algorithm uses images acquired during the first few minutes of the exam to triage patients to an abbreviated versus full MRI protocol. We conduct a retrospective reader study to show that this personalized scanning paradigm decreases scan time and cost while maintaining diagnostic performance.Introduction
Annual screening breast MRI is recommended in women at high risk of breast cancer and is being increasingly considered in women with a personal history of cancer or with dense breast tissue. A typical breast MRI protocol includes a dynamic contrast-enhanced (DCE) component, the workhorse of breast MRI interpretation, as well as several non-DCE sequences, which help the radiologist in only ~5% of cases and which add at least 10 minutes to scan time.1,2 Our group previously developed a DL model to triage breast MRIs according to their suspicion score using subtraction MIPs.3 Herein, we propose using this suspicion score for real-time mid-exam triage of patients to an AB-MR protocol versus a full MR protocol. To evaluate clinical impact of this personalized scanning paradigm, we conducted a reader study.Methods
This IRB-approved HIPPA-compliant retrospective study included consecutive contrast-enhanced screening breast MRs performed at two of our regional cancer care centers from January 2013-January 2019. Exams from these sites were selected since they were not used during the training or validation of the DL tool for Breast MRI Triage. Exams were excluded if they lacked standard axial post-contrast protocol, standard DICOM header labels, or necessary pathology follow-up. The radiology report BI-RADS score, pathology results, and tumor laterality information were extracted from the electronic medical record for all women. Cancer cases were defined as invasive or in situ disease diagnosed within 1 year of the MRI exam. To simulate implementation of a smart AB-MR paradigm (see Figure 1), our DL tool was used to retrospectively triage patients to the AB-MR versus full MR protocol. A DL suspicion score was generated for each MR exam. Exams with suspicion scores in the lowest quartile were reviewed by readers. Readers first reviewed the DCE sequences only and assigned a BI-RADS (AB-MR simulation score), the rest of the MR sequences were then unblinded and readers assigned a second BI-RADS (full MR simulation score). Readers were blinded to the radiology report, but encouraged to view all prior exams and reports. Readers were also blinded to the DL suspicion score. For exams where the DL suspicion score was not in the lowest quartile of suspicion, the radiology report BI-RADS was taken as the BI-RADS score (i.e. full protocol score). A range of smart AB-MR algorithmic cut-offs were then simulated such that the percent of exams triaged to AB-MR ranged from 0% to 25%. For example, for a 10% cutoff: the AB-MR BI-RADS Score was used for 0-10% lowest suspicion exams, the Full MR BI-RADS Score was used for the 11-25% of exams and the report BI-RADS was used for the 26-100% of exams. For each algorithmic cutoff, the sensitivity, specificity and positive predictive value were calculated with 95% confidence intervals, using a histopathology reference standard. McNemar’s chi-squared test was used to compare diagnostic accuracy of the full MRI protocol versus the smart AB-MR protocol with a 25% cutoff.Results
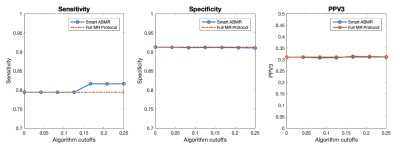
A total of 1,441 screening breast MRI exams were included in this study. This included 69 (4.7%) malignant exams and 1,372 (95%) benign exams based on a histopathology reference standard or one year of negative follow-up. In the reader study, the full MR protocol yielded a sensitivity, specificity and PPV3 of 79.4%, 91.2% and 31.0% respectively. When the smart AB-MR protocol was used with a cutoff of 25% (i.e. exams in the lowest quartile of suspicion triaged to AB-MR), sensitivity, specificity and PPV3 were 81.6%, 91.0% and 31.1% respectively. See Figure 2. There was no significant difference between diagnostic accuracy of the full protocol and smart AB-MR protocol (p = 0.5). There were five malignant exams, identified on the original clinical read, that landed in the DL tool’s lowest quartile of suspicion. Of these, two exams were correctly given a suspicious BI-RADS by readers on both the AB-MR and Full Protocol, and three cases were correctly given a suspicious BI-RADS on AB-MR, but were incorrectly downgraded to probably benign on the Full Protocol. Conversely, six benign cases correctly classified with the DL tool were incorrectly designated suspicious by readers on AB-MR and then were correctly downgraded to probably benign on the Full Protocol.Discussion
Our reader study demonstrates that a DL triage tool has the potential to process breast MRI images while the patient is on the scanner and triage up to 25% of exams to an AB-MR protocol while maintaining diagnostic accuracy. This would decrease scan time by at least 50% and would also likely reduce the radiologist’s interpretation time. It would require a reordering of the breast MR protocol (i.e. DCE sequences must be acquired first), but prior work indicates that the diagnostic quality of non-DCE sequences would be maintained post-contrast injection.4Conclusion
Our smart AB-MR protocol uses DL to triage 25% of exams to an AB-MR protocol without significant changes in diagnostic accuracy compared to the full protocol. This personalized scanning paradigm would decrease cost and decrease scan time compared to the full protocol without significant changes in diagnostic performance. Alternatively, it could be used as a safety check in centers that already offer AB-MR, averting situations where interpretating radiologists recommend the patient to return for additional breast MR sequences.Acknowledgements
No acknowledgement found.References
1. Mann R, Cho N, Moy L. Breast MRI: State of the Art. Radiology. 2019. 292:3, 520-536.2. Baxter GC, Selamoglu A, Mackay JW, Bond S, Gray E, Gilbert FJ. A meta-analysis comparing the diagnostic performance of abbreviated MRI and a full diagnostic protocol in breast cancer. Clin Radiol. 2021.3. Bhowmik A, Monga N, Belen K, Varela K, Sevilimedu V, Thakur S, Martinez D, Sutton E, Pinker K, Eskreis-Winkler S. Automated Triage of Normal Breast MRI Exams in High-Risk Women Using an Ensemble Deep Learning Model. In review.4. Dorrius MD, Dijkstra H, Oudkerk M, Sijens PE. Effect of b value and pre-admission of contrast on diagnostic accuracy of 1.5-T breast DWI: a systematic review and meta-analysis. Eur Radiol. 2014 Nov;24(11):2835-47.
DOI: https://doi.org/10.58530/2023/0185