0184
Screening abbreviated breast MRI with ultrafast imaging: prospective study results1Radiology, University of Pittsburgh, Pittsburgh, PA, United States, 2University of Chicago, Chicago, IL, United States
Synopsis
Keywords: Breast, Breast, Abbreviated Breast MRI
We report on the results of a prospective screening trial using abbreviated breast MRI with ultrafast dynamic contrast-enhanced imaging (3.5 seconds per time point) to screen for breast cancer in 166 women at any risk of developing breast cancer. The cancer detection rate was 24.1 per 1000 women while maintaining a specificity of 97.6%. The biopsy recommendation and abnormal interpretation rates were lower than in other published trials that did not include ultrafast imaging in their abbreviated protocol.Introduction
Abbreviated breast MRI (Ab-MRI) has been introduced as an alternative for screening women with dense breasts and at intermediate risk for developing breast cancer1. A multicenter trial2 showed that Ab-MRI had a higher cancer yield than digital breast tomosynthesis in women with dense breasts. However, some concerns remain about the possibility for high numbers of fall positives through breast cancer screening Ab-MRI3. In an Ab-MRI protocol, the high spatial resolution dynamic contrast-enhanced (DCE) series is typically reduced to one pre-contrast and one post-contrast acquisitions. The post-contrast time point is usually acquired so that the center of k-space is sampled roughly 90 seconds after contrast media administration. This timing allowed us to acquire an ultrafast DCE series for the first 60 seconds post-contrast while retaining the standard Ab-MRI scans. Breast ultrafast MRI has been shown to yield useful information for lesion detection and classification4-6. In this trial, most of the participants were women with dense breasts as identified by screening mammography (BI-RADS category C or D). Patients were recruited at community outreach events, or through physician referral. Participants without prior screening mammograms were enrolled in the study even if they were later found not to have dense breasts.Methods
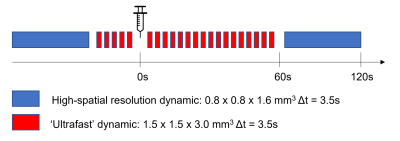
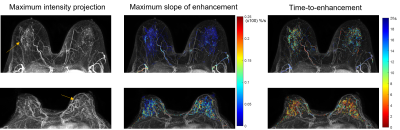
Patients were enrolled into an IRB-approved prospective trial. The Ab-MRI imaging protocol consisted of: calibration scans and localizers, a non-fat-suppressed T2-w series, and a DCE-MRI series acquired before and after administration of contrast media (0.1 mM/kg gadobenate dimeglumine or gadobutrol). Total acquisition time was under 10 minutes. The DCE series (Fig. 1) was made up of interleaved high spatial resolution T1-w images and an ultrafast series acquired for the first minute of post-contrast imaging with a temporal resolution of approximately 3.5 seconds. The DCE acquisitions were T1-weighted SPGR with cartesian sampling and fat-suppression. All scans were acquired at 3T with a 16-channel bilateral breast coil. Studies were interpreted according to the Breast Imaging Reporting and Data System (BI-RADS) as part of the routine breast MRI clinical workflow, including the ultrafast series which is part of the routine protocol at our institution.Results
166 patients underwent Ab-MRI from January 2017 to February 2022. Mean patient age was 51.8 years (range 24 – 74 years). Indication for Ab-MRI was dense breasts for 134 (81%) patients. 1 patient was included due to personal history of breast cancer (10 other patients also had dense breasts and a personal history of breast cancer). Breast density information was missing for 29 patients at the time of recruitment, and 2 patients with category B density were included in the study. The breakdown of Ab-MRI BI-RADS scores was: [0] incomplete – 3 (1.8%); [1] negative – 109 (65.7%); [2] benign – 45 (27.1%); [3] probably benign – 1 (0.6%); [4] suspicious – 6 (3.6%); [5] highly suggestive of malignancy – 2 (1.2%). The 3 patients with BI-RADS 0 received short term follow-up imaging, all resulting in BI-RADS 3 scores. Biopsy was recommended for 8 patients (4.8%). Of those 8, biopsy results were available for 6 patients, 3 were malignant (invasive ductal carcinoma), 2 benign and 1 atypical ductal hyperplasia which was upstaged to DCIS following surgical resection. The cancer detection rate was 24.1 per 1000 women. The abnormal interpretation rate was 7.2%. Follow-up imaging occurring 12+ months after Ab-MRI was available for 36 patients whose Ab-MRI was negative or had a benign finding. Follow-up imaging was normal for 35 of them, with 1 patient undergoing a benign biopsy based on follow-up imaging. 6-to-12-month follow-up imaging was available for an additional 18 patients with normal Ab-MRIs, with all 18 being normal (BI-RADS 1 or 2). Sensitivity (calculated based on the cases with follow-up imaging) was 100% and specificity was 97.6%. The positive predictive value (PPV1) – defined as the percentage of positive examinations that resulted in a cancer diagnosis within 1 year – was 44.4% (when defining BI-RADS scores 3, 4, and 5 as positive).Discussion
The breast cancer yield in our study was higher than that of a larger multi-center trial2, 24.1 per 1000 women vs 15.9. This is most likely due to the inclusion of women with a personal history of breast cancer (personal history was in the exclusion criteria for the EA1141 trial). Two of the cancers detected in this study were in women with personal history of breast cancer. Additional imaging (call-back or short-term follow-up) was required in 2.4% of women. This value is lower than that published in other trials (e.g. 7.5%2, 5.6%7 and 31.1%3). The biopsy recommendation rate (4.8%) was lower than in other studies (7%2 and 14%3) and higher than the 2.2% reported by Kwon et al7. The specificity of Ab-MRI with ultrafast imaging was high while maintaining 100% sensitivity. These results are in line with a previous study8 that showed that the addition of ultrafast imaging to Ab-MRI increases specificity.Conclusions
The results of this study confirm the value of Ab-MRI as a technique with high sensitivity for the detection of breast cancer. The addition of ultrafast MRI to Ab-MRI protocols may help increase their specificity and reduce the number of unnecessary biopsies, which is key to its wider adoption for breast cancer screening.Acknowledgements
This work was funded by the National Cancer Institute of the National Institutes of Health through grant : R01 CA218700References
1. Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB: Abbreviated breast Magnetic Resonance Imaging (MRI): First postcontrast subtracted images and maximum-intensity projection - A novel approach to breast cancer screening with MRI. J Clin Oncol 2014; 32:2304–2310.
2. Comstock CE, Gatsonis C, Newstead GM, et al.: Comparison of Abbreviated Breast MRI vs Digital Breast Tomosynthesis for Breast Cancer Detection among Women with Dense Breasts Undergoing Screening. JAMA - J Am Med Assoc 2020; 323:746–756.
3. Kennard K, Wang O, Kjelstrom S, et al.: Outcomes of Abbreviated MRI ( Ab-MRI ) for Women of any Breast Cancer Risk and Breast Density in a Community Academic Setting. Ann Surg Oncol 2014.
4. Mann RM, Mus RD, van Zelst J, Geppert C, Karssemeijer N, Platel B: A Novel Approach to Contrast-Enhanced Breast Magnetic Resonance Imaging for Screening. Invest Radiol 2014; 49:579–585.
5. Pineda FD, Medved M, Wang S, et al.: Ultrafast Bilateral DCE-MRI of the Breast with Conventional Fourier Sampling. Acad Radiol 2016; 23:1137–1144.
6. Abe H, Mori N, Tsuchiya K, et al.: Kinetic Analysis of Benign and Malignant Breast Lesions With Ultrafast Dynamic Contrast-Enhanced MRI: Comparison With Standard Kinetic Assessment. Am J Roentgenol 2016; 207:1159–1166.
7. Kwon M, Park KW: Breast Cancer Screening with Abbreviated Breast MRI : 3-year Outcome Analysis. 2021.
Figures