0153
The Patients’ Experience on Neuroimaging of Gliomas: A Cross-Sectional Survey Study1Radiology & Nucleaire Medicine, Amsterdam UMC location Vrije Universiteit Amsterdam, Amsterdam, Netherlands, 2Brain Tumor Center Amsterdam, Cancer Center Amsterdam, Amsterdam, Netherlands, 3Neuroscience, Amsterdam UMC location Vrije Universiteit Amsterdam, Amsterdam, Netherlands, 4Neurosurgery, Amsterdam UMC location Vrije Universiteit Amsterdam, Amsterdam, Netherlands, 5UCL institutes of Neurology and Healthcare Engineering, London, United Kingdom
Synopsis
Keywords: Tumors, Challenges, Patient experience
Glioma patient experience of MRI scans, repeated follow-up, and gadolinium-based contrast agents (GBCA) are unknown, despite the vulnerability of this patient group and relevant implications for clinics and science. This cross-sectional survey questioned 100 patients with primary brain tumors and found generally positive experiences with neuro-oncological scans. Age, diagnosis, and number of previous scans had little impact on the patient experience. However, women found MRI and intravenous injection significantly more uncomfortable. Also, patients would prefer GBCA-free MRIs if diagnostically equivalent. Patient knowledge towards GBCAs was limited and better information regarding GBCA and the MRI itself is needed.Introduction
Glioma patients usually receive several MRI scans per year as standard care. Research endeavors towards faster and more informative MRI protocols are ongoing1,2, but glioma MRI protocols remain lengthy and include gadolinium-based contrast agents (GBCA). The patient opinion on radiological care is largely unknown, despite the vulnerability of glioma patients and the aim of healthcare systems for shared decision making. This also has a negative impact on the planning of future MRI research lines.This study gains insight into the patient’s perspective on neuro-oncological MRI, frequency of follow-up, and use of GBCAs.
Methods
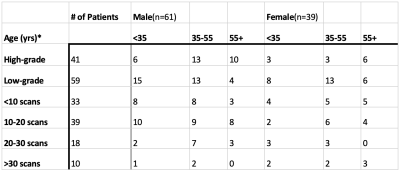
Participants and study designOne-hundred patients filled in a short survey after their MRI exam, 61 by male patients (mean age ± standard deviation (SD): 44 ± 14 years) and 39 by female patients (mean age ± SD 46 ± 13 years, table 1). Ninety-one patients had a histopathologically confirmed diagnosis and 9 patients were considered to have a slow growing low grade tumor after multidisciplinary discussion.
Analysis
Questions were analyzed to determine trends in patient experience regarding the MRI itself, frequency of follow-up, and the use of GBCAs. Subgroup analyses were performed on sex, glioma entity, age, and number of scans. Subgroup comparison was done using Pearson chi-square test and the Mann-Whitney U-test for categorical and ordinal questions, respectively. The significance level was set at P < 0.05.
Results
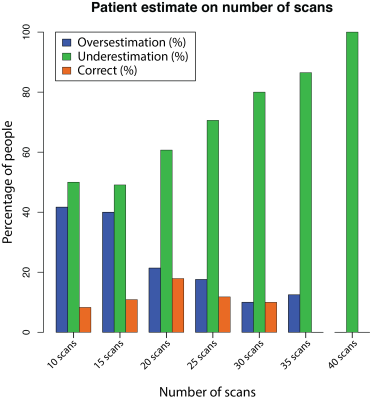
General burden of MRIPatients overall underestimated the number of scans they had undergone. An increase in the number of follow-up scans was associated with an increased underestimation of MRI burden (figure 1). When overestimation occurred, it was more marked than in cases of underestimation: 7.2 ± 7.7 compared to 4.8 ± 4.5 scans (mean±SD) respectively.
The general trend is that MRIs are not burdensome as visualized in fig. 2. The largest stress factor was fear of outcome/bad news (figure 2). Women had more symptoms during or directly after the MRI and found the MRI more annoying than males. Women also experienced more stress for bad news, the travel times, and experienced more stress in general. Age, diagnosis and number of previous scans had little impact on patients’ MRI perception.
Attitude towards GBCA injection
The majority of patients did not experience GBCA injections as burdensome (Figure 3). However, 40% had at least some irritation when receiving IV administration. Most patients would prefer, if diagnostically equivalent, GBCA-free MRI scans. Fifty-eight patients answered the additional question about possible adverse effects from GBCA and only 3 patients were aware of these.
Discussion
Patients with primary brain tumors expressed a generally positive attitude towards the current neuro-oncological MRI follow-up scheme in this monocentric survey at a tertiary academic center. However, patients would prefer GBCA-free MRI protocols, provided that diagnostic accuracy is maintained. Importantly, patient knowledge about potential adverse effects of GBCA was limited, and we identified women as less satisfied, while age, diagnosis, and number of previous scans had no impact on satisfaction.There was a positive memory bias by underestimating the number of scans they had undergone - a phenomenon deriving from a person’s inclination to marginalize unpleasant events and to remember them more favorably than they actually were3,4.
In the medical community there is a tendency to reduce scan frequency and duration. Arguments are costs, waiting lists, and the assumption that patients find the MRI uncomfortable and have difficulty complying5,6. However, our results showed that most patients did not experience the MRI procedure as burdensome and that the frequency of control scans is perceived as relevant to maintain - even for frequently scanned glioblastoma patients.
Overall, women found the MRI procedure more uncomfortable than men. This was characterized by experiencing the MRI procedure as more unpleasant, more often being afraid of bad news, and being more stressed about the travel times. These findings are in line with literature suggesting that women are twice as likely to experience stress and anxiety than men7. Sex should therefore be considered more when planning MRI scans. Being older, having a higher grade glioma or having had several scans does not have an impact on MRI experience and follow-up.
An estimated ~40% of all MRI scans in neuroradiology are GBCA-dependent. With the aim of shared decision-making, patient opinion on gadolinium should therefore be considered8. Our results show that most patients would opt for MRIs without GBCAs if considered diagnostically sound, supporting research in that direction. Patients, however, showed a lack of knowledge of GBCA including insufficient knowledge regarding possible adverse effects despite it being a frequently prescribed diagnostic agent. This lack of information can be interpreted as information asymmetry, an indicator of market failure, counteracting efforts to liberalize healthcare markets and thereby potentially keeping public healthcare costs - largely paid by tax-payer money - unnecessarily high.
Conclusion
The current study finds that patients with primary brain tumors have positive experiences towards the current neuro-oncological MRI procedures. Especially women, however, would support endeavors towards GBCA-free MRI diagnostics and shorter protocols. Approaches to reduce imaging frequency are not the patients’ priority (some even were worried not to be monitored closely enough). A lack of knowledge on GBCA indicates that shared decision-making remains an unreached goal in glioma imaging (and beyond).Acknowledgements
No acknowledgement found.References
1. Smith-Bindman, R. et al. Trends in Use of Medical Imaging in US Health Care Systems and in Ontario, Canada, 2000-2016. JAMA. 2019;322(9): 843–856.
2. Recht, M. P. et al. Optimization of MRI Turnaround Times Through the Use of Dockable Tables and Innovative Architectural Design Strategies. AJR Am. J. Roentgenol. 2019;212(4): 855–858.
3. Adler, O. & Pansky, A. Chapter 7 - A ‘rosy view’ of the past: Positive memory biases. in Cognitive Biases in Health and Psychiatric Disorders (eds. Aue, T. & Okon-Singer, H.) (academic press) 2020: 139–171.
4. Sedikides, C. & Green, J. D. Memory as a self-protective mechanism. Soc. Personal. Psychol. Compass 3, 1055–1068 (2009).
5. Mekle, R., Wu, E. X., Meckel, S., Wetzel, S. G. & Scheffler, K. Combo acquisitions: balancing scan time reduction and image quality. Magn. Reson. Med. 2005;55(5): 1093–1105.
6. Sartoretti, E. et al. Reduction of procedure times in routine clinical practice with Compressed SENSE magnetic resonance imaging technique. PLoS One 2019;14(4):, e0214887.
7. Remes, O., Brayne, C., van der Linde, R. & Lafortune, L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 2016;6(7): e00497.
8. Shared decision making. NHS England https://www.england.nhs.uk/personalisedcare/shared-decision-making/. Accessed October 2, 2022.
Figures