0101
Towards the understanding of the the role of Functional strength markers in Cartilage-Bone Cross Talk: a PET/MRI study in isolated PFJOA patients1Department of Radiology and Biomedical Imaging, University of California, San Francisco (UCSF), San Francisco, CA, United States, 2Department of Physical Therapy and Rehabilitation Science, University of California, San Francisco (UCSF), San Francisco, CA, United States
Synopsis
Keywords: Bone, PET/MR, SUV, T1rho, flexion strength, extension strength, patellofemoral OA, Cartilage-Bone-CrossTalk
In this exploratory study, we investigated standardized-uptake-values(SUV) from simultaneous bilateral PET-MRI, and individual joint loading in knees cross-sectionally in patients with isolated PFJOA. Additionally, to discover regions of colocalized changes in bone-cartilage interactions, we explored SUV interactions with cartilage biomarker T1rho relaxation values from high-resolution bilateral axial MAPSS. Strong negative correlations were between knee normalized isometric strength vs. maximum SUV in the lateral patella and medial trochlea, suggest higher degree of ongoing bone-remodelling combined with decreased knee flexion and extention strength. The existance of parallel higher trochlear bone remodelling and cartilage loss (disease progression) or vice-versa was also noted.
Introduction
Approximately one third of the adults with Osteoarthiritis (OA) over the age of 50, suffer from isolated patellofemoral-joint (PFJ)-OA1, causing significant pain and joint dysfunction and structural damage of patellar and trochlear cartilages. Behavior of isolated PFJOA often differs from tibiofemoral-joint-OA(TFJOA) or mixed-OA, especially in terms of pregression. Multicenter studies spanning years have shown knees developing mixed-OA/structural damage, are more likely to start as isolated in PFJ2. Based on the OA model proposed by Burr et. al3, it can be hypothesized that remodelling of patellar/trochlear subchondral and trabecular bone caused by repetitive joint loading could be a precursor of bone-cartilage crosstalk. Bone-cartilage interactions can subsequently increase vascularization of the deep cartilage layers, finally breaking down the cartilage collagen network and resulting in proteoglycan loss depicted as cartilage damage4. Well documented morphological, compositional, and metabolic imaging tools5, are available and have been explored in isolation, for understanding these complex pathophysiological possibilities. In this preliminary work, we investigated standardized-uptake-values(SUV) from Positron-Emission-Tomogrphy (PET), and individual joint loading in knees cross-sectionally in patients with isolated PFJOA. Additionally, to discover regions of colocalized changes in bone-cartilage interactions, we explored SUV interactions with cartilage biomarker6 T1rho relaxation values.Methods
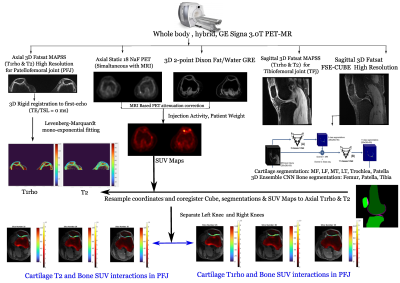
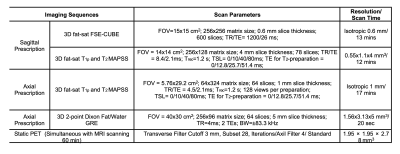
Ten patients (age: 50±11.41 years; sex: four females, one gender nonbinary; BMI: 24.45±2.34) with isolated PFJOA in one or both knees, provided written consents for this IRB-approved ongoing study. Patient inclusion was verified by a radiologist trained and expert in MSK. WORMS score in patellar and trochlear compartments were reviewed for each patient. Patients having any history of traumatic-knee-injury or presence of tibiofemoral involvement, were excluded from the study. Patients underwent simultaneous 18NaF PET-MRI scanning in a 3.0T whole-body, hybrid, GE-Signa PET-MRI scanner (GE Healthcare, Waukesha, WI) for bilateral morphological, compositional, and metabolic knee imaging (Figure 1). Bilateral knee sagittal 3D fat-sat CUBE and axial high-resolution MAPSS were acquired simaltanoeusly with axial PET-scans for each patient (Table 1). The axial high-resolution T1rho maps from axial-MAPSS7 were obtained using a 3D rigid-registration and Levenberg-Marquardt mono-exponential fitting algorithm7. 3D 2-point-Dixon images were utilized for MRI-based static-PET attenuation correction8 followed by SUV maps calculation utilizing injection activity and patient weight. Bilateral trochlear and patellar bones and cartilage volumes were autoamatically segmented on the CUBE images using two separate ensemble 3D V-Net architectures910. The SUV maps and segmentations were resampled and registered to the T1rho images. An automated algorithm was formulated to subdivide the trochlea and patellar bones into medial and lateral aspects and the trochlear and patellar cartilage volumes into deep-medial, deep-lateral, superficial-medial, and superficial-lateral regions. Knee flexion and extension isometric strength were measured using a HUMAC NORM dynamometer (Computer Sports Medicine, inc) and were normalized for patient weight11. Pearson correlations were computed between knee flexion and extension normalized isometric strength (Nm/Kg) and compartmental maximum SUV values in the trochlea and patella bone (R-Studio-Core, 2022.07.2). Additionally, Pearson correlations were computed between T1rho values of patellar and trochlear cartilage compartments. Statistical significance was set at p<0.05.Results and Discussion
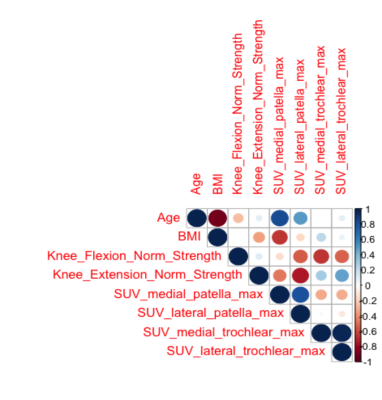
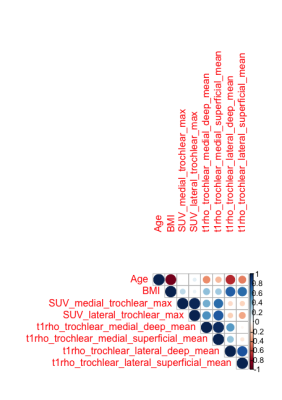
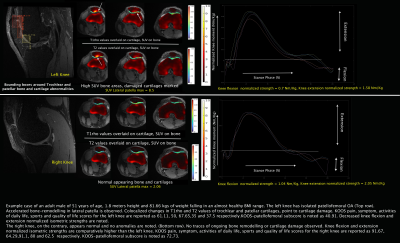
Strong negative correlations (R = -0.84, p<0.05) were observed between knee extension strength and maximum SUV in the lateral patella (Figure-2). A moderate negative correlation (R = - 0.59, p<0.05) was also observed between knee flexion trength and maximum SUV in the medial trochlea. Additionally moderate positive correlations were found between maximum SUV in the medial and lateral regions of the trochlear bone and the deep medial and superficial layers of the trochlear cartilage respectively, R = 0.78, 0.72, p<0.05 (Figure-3). As an example, patient #1 had diagnosed unilateral PFJOA, with notable increased SUV in the patella of the knee with OA compared to the contralateral patella (Figure-4). These findings suggest higher degree of ongoing bone-remodelling correlates with decreased knee flexion and extention strength. Whether the loss in knee strength causes bone remodelling or the opposite, is difficult to determine. Whether there exists distinct phases of gait stance, which can correlate better with metabolic bone remodelling, remains to be explored. The crosstalk pattern in isolated PFJOA is expected to be complex in terms of regional involvements. The existance of parallel higher trochlear bone remodelling and cartilage loss (disease progression) is also noticed. The sample size is limited for generalizations on the direct relationships between compositional, biomechanical, and metabolic aspects, but conveys feasible potential in this exploratory analysis. The striking differences in terms of maximum SUV values, bone remodelling and cartilage loss reflects in the gait curves ultimately resulting into difference in isometric strengths in the knees.Conclusion
In this study, we present one of the first studies to explore bone remodelling in isolated PFJOA in correlation with knee isometric strength and cartilage compartmental T1rho. Decreased knee flexion and extension strength were noted in correlation with accelerated bone-remodelling in medial trochlea and lateral patella, suggesting complex regional interactions and motivates follow up for longitudinal disease trajectories. Moderate positive correlations point to colocalized changes in medial-lateral trochlear bone and adjacent medial deep and superficial trochlear cartilage suggesting crosstalks in between them. A possible understanding of whether the compositional vs. metabolic and biomechanical vs. metabolic relationships have a mediated effect on one another seems to be the next possible step towards decoding the isolated PFJOA progression with inclusion of more subjects.Acknowledgements
This project was supported by R01AR079647 (NIH)References
1. Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, Kelly-Hayes M, Wolf PA, Kreger BE, Kannel WB. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84(3):351-8. PubMed PMID: 8129049.2. Stefanik JJ, Guermazi A, Roemer FW, et al. Changes in patellofemoral and tibiofemoral joint cartilage damage and bone marrow lesions over 7 years: The Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2016;24(7):1160-1166. doi:10.1016/j.joca.2016.01.981
3. Burr DB, Gallant MA. Bone remodelling in osteoarthritis. Nat Rev Rheumatol. 2012;8(11):665-673. doi:10.1038/nrrheum.2012.130
4. Findlay DM, Kuliwaba JS. Bone-cartilage crosstalk: a conversation for understanding osteoarthritis. doi:10.1038/boneres.2016.28
5. Tibrewala R, Pedoia V, Bucknor M, Majumdar S. Principal Component Analysis of Simultaneous PET-MRI Reveals Patterns of Bone–Cartilage Interactions in Osteoarthritis. Journal of Magnetic Resonance Imaging. 2020;52(5):1462-1474. doi:10.1002/jmri.27146
6. Stahl R, Luke A, Li X, et al. T1rho, T2 and focal knee cartilage abnormalities in physically active and sedentary healthy subjects versus early OA patients - A 3.0-Tesla MRI study. Eur Radiol. 2009;19(1):132-143. doi:10.1007/s00330-008-1107-6
7. Han M, Tibrewala R, Bahroos E, Pedoia V, Majumdar S. Magnetization-prepared spoiled gradient-echo snapshot imaging for efficient measurement of R2-R1ρ in knee cartilage. Magn Reson Med. 2022;87(2):733-745. doi:10.1002/mrm.29024
8. Leynes AP, Yang J, Shanbhag DD, et al. Hybrid ZTE/Dixon MR-based attenuation correction for quantitative uptake estimation of pelvic lesions in PET/MRI. Med Phys. 2017;44(3):902-913. doi:10.1002/mp.12122
9. Astuto B, Flament I, Namiri NK, et al. Automatic deep learning–assisted detection and grading of abnormalities in knee MRI studies. Radiol Artif Intell. 2021;3(3). doi:10.1148/ryai.2021200165
10. Caliva F, Iriondo C, Martinez AM, Majumdar S, Pedoia V. Distance Map Loss Penalty Term for Semantic Segmentation. Published online August 9, 2019. http://arxiv.org/abs/1908.03679
11. Teng HL, MacLeod TD, Link TM, Majumdar S, Souza RB. Higher knee flexion moment during the second half of the stance phase of gait is associated with the progression of osteoarthritis of the patellofemoral joint on magnetic resonance imaging. Journal of Orthopaedic and Sports Physical Therapy. 2015;45(9):656-664. doi:10.2519/jospt.2015.5859
Figures