0089
A linear model analysis of pain sensitisation in knee osteoarthritis assessed by MRI in relation to the blood biomarker thrombospondin-41Molecular and Clinical Sciences, St George's, University of London, London, United Kingdom, 2Infection & Immunity, St George's, University of London, London, United Kingdom, 3Radiology, St George's University Hospital Foundation Trust, London, United Kingdom, 4Infection & Immunity, St George's University Hospital Foundation Trust, London, United Kingdom, 5Rheumatology, St George's University Hospital Foundation Trust, London, United Kingdom
Synopsis
Keywords: Osteoarthritis, Degenerative, Pain
We investigated how pain in knee osteoarthritis (OA) relates to physical damage, clinical parameters, pain sensitisation and serum levels of thrombosponin-4 (TSP4). Across all patients (mild and advanced OA), the number of osteophytes (nOst) and TSP4 levels are significant factors in determining pain levels, with BMI and HADS the strongest factors. Grouping the patients according to low and high TSP4 levels, suggests a TSP4 phenotype that relates to central sensitisation. For high TSP4, pain pressure thresholds are a significant factor in reported knee pain in addition to HADS, BMI and physical damage.INTRODUCTION
For patients with knee osteoarthritis (OA), pain presents as a major clinical feature and disabling symptom. Structural damage observed by MRI has long been linked to knee pain1, with worsening damage linked to disease progression2. However, large increases in joint pain can occur with little change in structural damage3. Such pain changes, as well as increased pain sensitisation in body regions not associated with OA, are being linked to the mechanism of central sensitisation as a general feature of osteoarthritis2,4. Thrombospondin-4 (TSP4) is a candidate for mediating pain sensititation5 and is highly expressed in human OA cartilage6. In this study we have used a mixed General Linear Model (GLM) to assess which factors of knee damage (by MRI) contribute most to the variation in reported pain and whether serum TSP4 levels are a factor related to pain sensitisation.METHODS
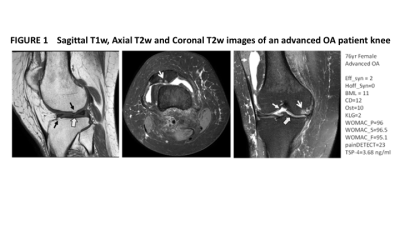
Subjects. A retrospective analysis was performed on 90 patients with clinical assessment of Mild OA (usual care with analgesics) or Advanced OA (scheduled for knee replacement surgery). MRI of the most affected knee comprised sagittal T1w (TE 15ms TR 600ms) and axial and coronal intermediate weighted (IW, TR 5000ms, TE 30ms) with fat-suppression. The MRI osteoarthritis score (MOAKS) was used to evaluate damage. In our mixed GLM we include scores for Hoffa and Effusion Synovitis (Hoff_Syn, Eff_Syn), and total number of bone marrow lesions (nBML), cartilage damaged regions (nCD) and osteophytes (nOst). Quantitative Sensory Testing (QST) of the knee and patella, as well as contralateral knee, wrist and malleolus was performed with an algometer. Pain score assessment was by Western Ontario and McMasters Universities Arthritis Index for pain (WOMAC_P) and painDETECT questionnaire7. Serum TSP4 was determined by a standard ELISA kit. Age, gender, BMI and HADS were incorporated as potential co-variates.Statistical analysis. For correlations, TSP4 was log-transformed due to its skewed distribution. Pearson’s correlation was used to assess which of the measured factors were correlated with WOMAC_P. Strategies were applied to prevent overfitting with the GLM. PCA was applied to QST measures to create a single score (QST_PC) representing a whole-body assessment of pain pressure threshold. A binary variable TSP4_M, was set to 0 for TSP4 < median, equal to 1 otherwise. Similarly, PDhigh was set to 1 for painDETECT >= 19 to represent the pain sensitised group, and otherwise set equal to 0. A mixed GLM was set up with WOMAC_P the target, with BMI, HADS and QST_PC as initial key covariates, and TSP4_M a factor. Each MRI MOAKS parameter was tested individually to determine the parameter with greatest contribution to WOMAC_P variability, which was then kept in the model. Finally, Gender was tested for significance and kept in for p<0.05, and any parameters with p<0.05 then removed. Group comparisons using Mann-Witney and GLM assessments were made for various subgroups. IBM SPSS v28 was used for all analyses.
RESULTS
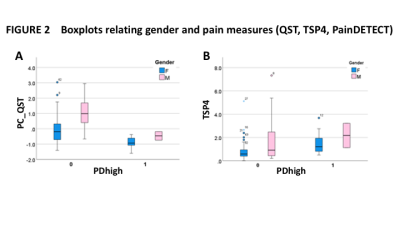
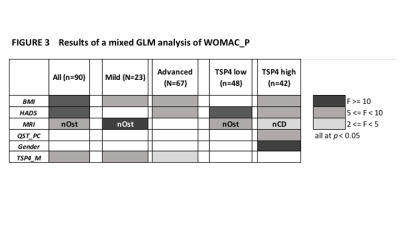
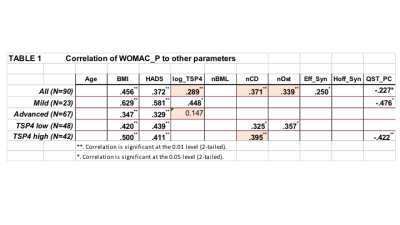
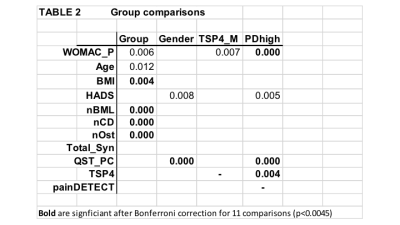
Fig. 1 shows an example set of MRI and MOAKS features of damage. There were highly significantly correlations of WOMAC_P with BMI and HADS across all data and sub-groups, and for logTSP4 across all data and the mild OA group. nBML was not correlated with WOMAC_P for any grouping, with various correlations for the other MOAKS parameters and with QST. After covarying for Age, BMI and HADS, we found nCD, nOst and TSP4 levels were the most significant factors determining WOMAC_P. Subgroup comparisons are shown in Table 2 and of note are that: QST is Gender dependent; WOMAC_P is significantly different between TSP4_M groups for no difference in MRI detected damage; pain sensitised grouping shows no difference in damage scores, but is different for WOMAC_P, QST and TSP4. Figure 2 demonstrates high pain pressure thresholds in men compared to woman independently of pain sensitisation (Fig. 4A); significantly higher levels of TSP4 in patients who are sensitised according to painDETECT criteria with a trend for TSP4 to be higher in men (Fig. 4B). The mixed GLM is consistent with these previous analyses and suggests the presence of a phenotype relating to TSP4 levels (Fig. 3): subjects with low TSP4 experience pain that is predominantly modulated by their depression score and physical damage; patients with high TSP4 with pain significantly related to sensitisation as well as physical parameters of damage.DISCUSSION
Our analysis suggests that TSP4 levels are an independent predictor of knee pain in osteoarthritis as well as an objective biomarker that could stratify patients to aid appropriate treatment. Stratifying patients according to clinical criterion of being mild or advanced OA, shows that BMI and TSP4 are consistent factors that determine pain. For mild OA, the significance of nOst suggests development of physical damage modulates pain, but for advanced OA, HADS is a significant factor but surprisingly, pain no longer covaries with physical damage. With TSP4 stratification, physical damage is always significant, and in the low TSP4 patient group, pain variance predominantly varies with depression, and the high TSP4 patient group pain is strongly related to QST suggesting central sensitisation. In conclusion our data suggests TSP4 is a marker of pain sensitisation with potential to aid patient stratification for appropriate treatment.Acknowledgements
Supported by the Rosetrees’ Trust (Grant number M11-F3), the Wellcome Trust Institutional Support Fund (ISSF) (Grant number 204809/16/Z) and the National Institute for Health Research (NIHR) Clinical Research Network.References
1. Yusuf E et al. Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann Rheum Dis 2011;70:60–67. doi:10.1136/ard.2010.131904.
2. Sofat N et al. Biomarkers in Painful Symptomatic Knee OA Demonstrate That MRI Assessed Joint Damage and Type II Collagen Degradation Products Are Linked to Disease Progression. Front Neuroscience. 2019;13:Article 1016. doi: 10.3389/fnins.2019.01016
3. Bacon K et al. Does cartilage loss cause pain in osteoarthritis and if so, how much? Ann Rheum Dis 2020;79:1105–1110. doi:10.1136/annrheumdis-2020-217363
4. Neogi et al. Association of Joint Inflammation With Pain Sensitization in Knee Osteoarthritis: The Multicenter Osteoarthritis Study. ArthritisRheumatol. 2016 March ; 68(3): 654–661. doi:10.1002/art.39488.
5. Kim D-S et al. Thrombospondin-4 Contributes to Spinal Sensitization and Neuropathic Pain States. The Journal of Neuroscience, 2012;32:8977– 8987.
6. Kuttapitiya A et al. Microarray analysis of bone marrow lesions in osteoarthritis demonstrates upregulation of genes implicated in osteochondral turnover, neurogenesis and inflammation. Ann Rheum Dis 2017;76:1764–1773. doi:10.1136/annrheumdis-2017-211396.
7. Moreton BJ et al. Pain Phenotype in Patients With Knee Osteoarthritis: Classification and Measurement Properties of painDETECT and Self-Report Leeds Assessment of Neuropathic Symptoms and Signs Scale in a Cross-Sectional Study. Arthritis Care & Research. 2015;667:519 –528. DOI 10.1002/acr.22431.
Figures