0071
Analyzing the Spatially-Resolved Performance of mpMRI for Detection of Prostate Cancer using a Prostate Sector Map1Department of Radiological Sciences, David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA, United States, 2Department of Diagnostic and Therapeutic Radiology, Ramathibodi Hospital, Bangkok, Thailand, 3Department of Medicine Statistics Core, University of California, Los Angeles, Los Angeles, CA, United States, 4Department of Urology, David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA, United States
Synopsis
Keywords: Data Analysis, Multimodal
Multiparametric MRI (mpMRI) has shown a marked impact on prostate cancer (PCa) diagnosis, but the understanding of the spatial distribution of tumors and the correlation between tumor location and mpMRI performance is still limited. The purpose of this study was to determine the performance of mpMRI for PCa detection and visualize the results on a prostate sector map described by Prostate Imaging Reporting and Data System (PI-RADS) v2.1. Also, this study aimed to investigate the association between mpMRI performance and tumor location in the prostate.Introduction
Multiparametric MRI before prostate biopsy in at-risk men is rapidly becoming the standard of care in clinical practice 1,2. However, it is crucial to investigate the accuracy and limitation of mpMRI for PCa detection. Whole-mount histopathology (WMHP), which can be prepared after radical prostatectomy, is the ideal reference standard for correlating individual histopathologically-confirmed PCa lesions to mpMRI findings to estimate mpMRI performance for tumor detection. Previously, several studies have examined the performance of mpMRI based on the tumor's pathological and spatial characteristics compared to WMHP 3-6. However, the spatial characteristics of PCa lesions associated with their detection/missing rate on mpMRI were not fully understood. The purpose of this study is to 1) analyze the spatially-resolved performance of mpMRI for detecting PCa lesions using a standard prostate sector map described in PI-RADS v2.1 and 7; 2) investigate the association between spatial location and detection rate of PCa lesions with different pathology specifications.Method
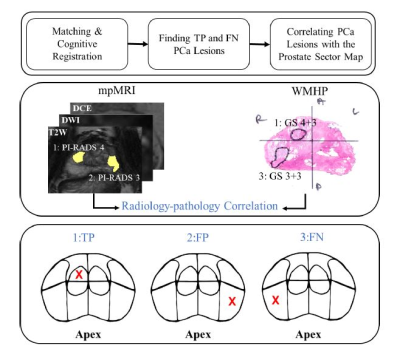
This HIPAA-compliant study was approved by the local institutional review board of our local institute with a waiver of informed consent. The study group for this single-institution observational study was composed of 931 consecutive men who underwent mpMRI prior to robotic-assisted radical prostatectomy (RALP) between 2010 and 2022. All suspicious lesions were contoured within the prostate by abdominal imaging fellows, confirmed by board-certified genitourinary (GU) radiologists, and manually mapped to the 41-segment PI-RADS v2.1 prostate sector map. The GU pathologist delineated all PCa lesions on WMHP and determined the pathological characteristics of the tumor.GU radiologists and pathologists re-reviewed each previously detected and graded lesion on WMHP and mpMRI and collectively determined concordance in the monthly radiologic-pathologic match meetings (Figure 1). A lesion that was detected on mpMRI (PI-RADS score ≥ 3) and WMHP was labeled as true positive (TP), and its sectors were recorded based on the appearance on mpMRI. The PCa lesions that were shown on WMHP but were not detected on mpMRI were classified as false negative (FN) lesions, and their sectors were assigned based on their appearance on WMHP. The mpMRI lesions were categorized as false positives (FP) if there is no corresponding lesion on WMHP. Collecting all information yielded the total number of TP, FP, and FN PCa lesions in each segment of the sector map. The guidelines issued by the International Society of Urological Pathology (ISUP) were used for the grading of prostate cancer, and clinically significant PCa was defined as a lesion with an ISUP grade of 2 or higher 8. The index lesion was defined as the PCa lesion with the highest ISUP grad or the largest size or both.
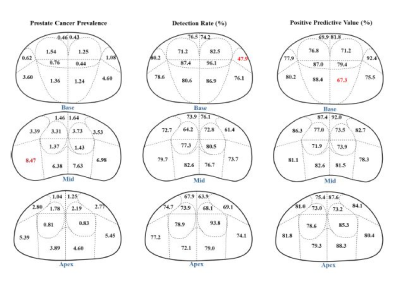
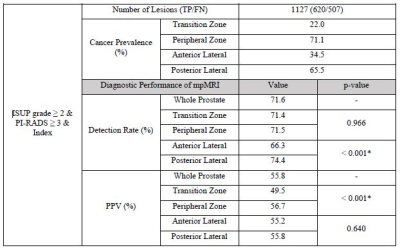
We used detection rate (DR), and positive predictive value (PPV) maps to identify hot spots on mpMRI with high cancer prevalence (CP), low DR, and low PPV values for PCa tumors with different pathological characteristics. To calculate CP, the number of lesions in each region of the sector map was divided by the total number of PCa lesions (TP+FN) stratified by pathologic characterization. DR and PPV were computed as TP/TP+FN and TP/TP+FP, respectively. Moreover, the correlation between mpMRI sensitivity in terms of DR and PPV and the location of PCa tumors on the prostate sector map was determined using a chi-square test.
Results
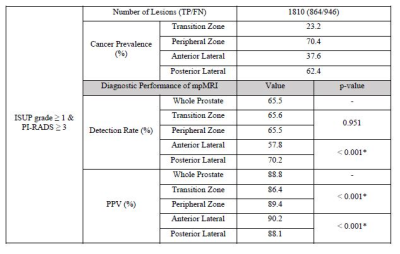
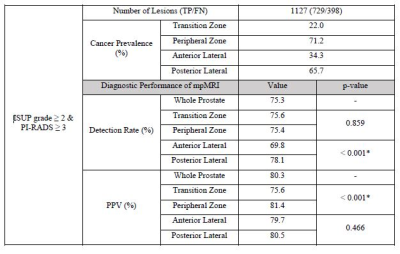
A total of 1810 PCa lesions (TP and FN) were identified in 931 patients at WMHP. Overall, the majority of PCa lesions with ISUP ≥ 1 or 2 were located on the PZ with a ratio of 3:1. The proportion of clinically significant (cs)PCa lesions increased by 50% in the posterior lateral prostate compared to that in the anterior region. Tables 1, 2, and 3 indicate the diagnostic performance of mpMRI for PCa lesions with ISUP ≥ 1, and 2 and for csPCa index tumors, stratified by prostate zones, respectively. As seen, for all three categories of tumors investigated in this study, DR in the posterior lateral region is significantly higher compared to that in the anterior region (p<0.001), while PPV in TZ is significantly lower than that in PZ (p<0.001). Figure 2 illustrates the CP, DR, and PPV maps for csPCa lesions. As shown, the performance of mpMRI for PCa diagnosis varied across sectors.Conclusion and Discussion
We studied the spatial characteristics of PCa lesions associated with mpMRI detection in correlation with WMHP using the largest dataset to date. The prostate sector map described by PI-RADS v2 was used as a template to visualize mpMRI performance in terms of CP, DR, and PPV for PCa lesions with various pathology specifications. Overall, mpMRI successfully detected two-thirds of tumors with ISUP ≥ 1 (DR of 66%). The detection rate of mpMRI significantly improved for csPCa and index csPCa tumors (DR of 75% and 72%, respectively, p<0.001 for both categories). However, the PPV of mpMRI for csPCa (80%) and index csPCa (56%) tumors decreased significantly compared to the tumors with ISUP ≥ 1 (89%) (p<0.001 for both categories). In a cohort of 931patients with mpMRI and WMHP with per lesion sector-based detection mpMRI was the best in the PZ and least in the anterior TZ; attention to these sectors may further improve PCa diagnosis.Acknowledgements
This work was supported in part by the National Institutes of Health R01-CA248506 and funds from the Integrated Diagnostics Program, Departments of Radiological Sciences and Pathology, David Geffen School of Medicine, UCLA.References
[1] Washino S, Kobayashi S, Okochi T, et al. Cancer detection rate of prebiopsy MRI with subsequent systematic and targeted biopsy are superior to non-targeting systematic biopsy without MRI in biopsy na€ıve patients: a retrospective cohort study. BMC Urol 2018;18:51.
[2] Faria R, Soares MO, Spackman E, et al. Optimising the diagnosis of prostate cancer in the era of multiparametric magnetic resonance imaging: a cost-effectiveness analysis based on the prostate MR imaging study (PROMIS). Eur Urol 2018;73:23–30.
[3] Johnson DC, Raman SS, Mirak SA, et al. Detection of Individual Prostate Cancer Foci via Multiparametric Magnetic Resonance Imaging. Eur Urol 2019;75:712–720.
[4] Wibulpolprasert P, Raman SS, Hsu W, et al. Detection and Localization of Prostate Cancer at 3-T Multiparametric MRI Using PI-RADS Segmentation. AJR 2019; 212: W122-W131.
[5] Wibulpolprasert P, Raman SS, Hsu W, et al. Influence of the Location and Zone of Tumor in Prostate Cancer Detection and Localization on 3-T Multiparametric MRI Based on PI-RADS Version 2. AJR 2020;214:1101-1111.
[6] Zabihollahy F, Raman SS, Wibulpolprasert P, et al., Localization of Prostate Cancer at 3-T Multiparametric Magnetic Resonance Imaging using Prostate Sector Map. ISMRM 2022, London, UK, 2022.
[7] American College of Radiology. PI-RADSTM Prostate Imaging- Reporting and Data System. ACR; 2019 https://www.acr.org/-/media/ACR/Files/RADS/Pi-RADS/PIRADS-V2-1.pdf.
[8] Egevad L , Delahunt B, Srigley JR 4, Samaratunga H. International Society of Urological Pathology (ISUP) grading of prostate cancer - An ISUP consensus on contemporary grading. APMIS. 2016;124(6):433-5.
Figures