0066
Anatomically Accurate In vitro Model of the Liver for 4D Flow MRI Validation1Mechanical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 2Radiology, University of Wisconsin-Madison, Madison, WI, United States, 3Radiology, Universität zu Lübeck, Lübeck, Germany, 4Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 5Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States, 6Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Keywords: Liver, Modelling
4D flow MRI can be used to assess hemodynamics in the hepatic circulation system. This study presents a framework for in vitro hemodynamic evaluation of hepatic flow. One patient-specific in vitro model was created representing an anatomically realistic portal vein and hepatic artery and connected to a physiologic flow loop. The model was imaged with 4D flow MRI to assess hemodynamics. Altering hepatic artery and left gastric vein resistance changed flow proportions and velocities in the portal vein, highlighting the benefit of using in vitro modeling for systematic evaluation of 4D flow MRI in the liver.Introduction
Hemodynamic analysis can improve the understanding of liver pathologies since changes in liver flow are often characteristic of specific disease1-4. 4D flow MRI is a quantitative imaging technique that allows for comprehensive assessment of blood flow in many vascular territories5. 4D flow MRI shows promise in assessing 3D hemodynamics in patients with various pathologies of the hepatic circulation system; however, one of its main limitations is lengthy scan times, limiting its use as a clinical diagnostic tool1-4,6. As a result, research has focused on novel acquisition and reconstruction schemes to reduce 4D flow MRI scan times, but quantitative validation remains a challenge. In vitro flow models allow for systematic evaluation of 4D flow MRI performance in anatomically realistic geometries with physiological flow that can be analyzed with higher resolution flow methods, like particle image velocimetry (PIV)7. The goal of this study was to develop an MRI and PIV compatible flow phantom of the hepatic circulation system to evaluate 4D flow MRI performance.Methods
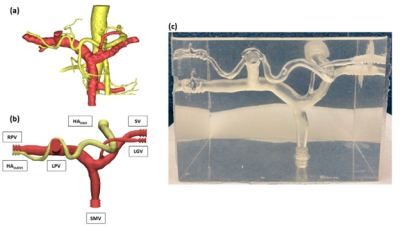
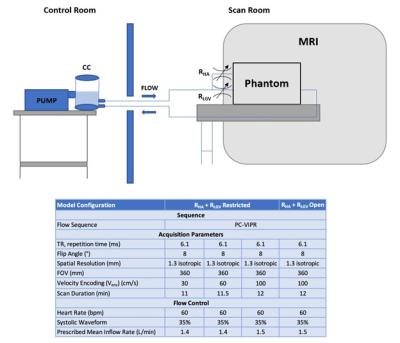
In this HIPAA compliant study, one patient underwent abdominal MRI following an IRB-approved protocol. 3D contrast enhanced-MRA was used for segmentation of the portal vein and hepatic artery and used to construct an the flow model using a hybrid additive manufacturing technique8. The model included the hepatic artery (HA), superior mesenteric vein (SMV), splenic vein (SV), left gastric vein (LGV), portal vein (PV), right portal vein (RPV) and left portal vein (LPV). Resistance valves were included in the hepatic artery (RHA) and left gastric vein (RLGV) to alter flow delivered to each model branch (Figure 1).The model was connected to a flow loop consisting of a pulsatile pump (BDC Labs), compliance chamber and resistance valves, and scanned on a 3.0T clinical MRI system (Signa Premier, GE Healthcare). Inflow rate was controlled by the pump. 3D flow dynamics were measured for different flow scenarios using a radially undersamped 4D flow sequence, PC-VIPR, and three different velocity encoding settings (Venc)9. ECG gaiting necessary for time-resolved acquisition was achieved using pump signal output. Fluid in the loop consisted of a blood-mimicking solution of water and glycerol that matched the refractive index of the model for PIV compatibility. Data analysis was performed in Ensight (Ansys, Inc). A schematic of the experimental setup and acquisition parameters are shown in Figure 2.
Results
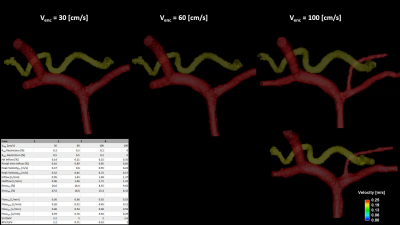
4D flow MRI data were successfully obtained for 4 different flow scenarios (Figure 3). Peak velocities ranged from 0.22-0.60 m/s and 0.32-0.57 m/s in the PV and HA, respectively, representing physiological values1-4. Partial occlusion of the HA increased peak velocities while decreasing the proportion of HA inflow. This diverted more flow to the PV, increasing flow velocities in the anatomical portal vein.The 4D flow MRI data results are re-summarized in in Figure 3. PV and HA inflow and outflow errors were analyzed following the conservation of mass principle. Errors were defined as the difference between total flow in all inlets and outlets with respect to portal vein flow. Errors ranged from 9-24% and 8-48% in the PV and HA, respectively. Higher errors were associated with lower Venc setting.
Discussion
This study utilized a patient-specific, anatomically accurate in vitro model of the hepatic portal system for hemodynamic analysis under controlled flow conditions. A Venc of 100 cm/s sufficiently captured flow in all vessels where inflow and outflow errors agree with previously published studies validating the consistency of 4D flow MRI3.As the HA and LGV are restricted, more flow is forced through the PV, increasing PV flow velocities. Flow acceleration in the HA was observed as HA diameter decreases. Peak velocities in the HA suggest that restriction also increases flow velocity in the HA. Fine tuning RHA and RLGV could be used to simulate the effects of physiologic and pathological conditions (meal challenge, cirrhosis) or render larger velocity differences between PV and HA for dual-Venc 4D flow applications. As Venc was decreased, conservation errors in the PV and HA increased, presumably due to aliasing.
Flow in the SMV was approximately twice the flow in the SV, which is consistent with physiologic flow in the PV3. Without restriction, flow in the RPV is twice that in the LPV. This changes with increased HA and LGV restriction, where LPV flow dominates RPV flow 2:1, suggesting restriction also affects PV outflow. Complete occlusion of the LGV was achieved at RLGV= 50% without negatively impacting flow in the SV, SMV or HA. This suggests additional resistive components can be included in the PV outflow tract to simulate embolism of the RPV or LPV without shunting the other vascular beds.
All cases configured the LGV as an inflow tract. The LGV could be configured as an outflow tract to simulate the effects of flow reversal in the LGV that result from portal hypertension10.
Conclusion
This study utilized a patient-specific MRI and PIV compatible phantom of the hepatic artery and portal vein to model hepatic circulation hemodynamics. Phantom hemodynamics were visualized and quantified using 4D flow MRI. Hemodynamics were altered by tuning vessel resistance valves, highlighting the benefit of using an in vitro modeling approach for systematic evaluation of 4D flow MRI in the hepatic portal system.Acknowledgements
The authors wish to acknowledge the NIH (R01 DK125783, R01 DK126850-01) for supporting this study, as well as GE Healthcare which provides research support to the University of Wisconsin.References
1. Oechtering TH, Roberts GS, Panagiotopoulos N, et al. Clinical application of 4D flow MRI in the portal venous system. Magn Reson Med Sci. 2022; 21(2):340-353.
2. Oechtering TH, Roberts GS, Panagiotopoulos N, et al. Abdominal applications of quantitative 4D flow MRI. Abdom Radiol. 2022; 47:3229-3250.
3. Roldan-Alzate A, Frydrychowicz A, Niespodzany E, et al. In vivo validation of 4D flow MRI for assessing hemodynamics of portal hypertension. J Magn Reson Imaging. 2013;37:1100-1108.
4. Roldan-Alzate A, Frydrychowicz A, Said A, et al. Impaired regulation of portal venous flow in response to a meal challenge as quantified by 4D flow MRI. J Magn Reson Imaging. 2016;42:1009-1017.
5. Markl M, Frydrychowicz A, Kozerke S, et al. 4D flow MRI. J Magn Reson Imaging. 2012;36(5):1015-1036.
6. Stankovic Z, Fink J, Collins JD, et al. K-t GRAPPA-accelerated 4D flow MRI of liver hemodynamics: influence of different acceleration factors on qualitative and quantitative assessment of blood flow. Magn Reson Mater Phy. 2015;28:149-159.
7. Rutkowski D, Medero R, Ruesink T, et al. Modeling physiological flow in Fontan models with four-dimensional flow magnetic resonance imaging, particle image velocimetry, and arterial spin labeling. J Biomech Eng. 2019;141(12):121004.
8. Ruedinger K, Medero R, Roldan-Alzate A. Fabrication of low-cost patient specific vascular models for particle image velocimetry. Cardiovasc Eng Tech. 2019;10(3):500-507.
9. Johnson KM, Lum DP, Turski PA, et al. Improved 3D phase contrast MRI with off-resonance corrected dual echo VIPR. Magn Reson. Med. 2008;60(6):1329-1336.
10. Motosugi U, Roldan-Alzate A, Bannas P, et al. Four-dimensional flow MRI as a marker for risk stratification of gastroesophageal varices in patients with liver cirrhosis. Radiology. 2019;290(1):101-107.
Figures