5053
SAR Considerations of MRI Patients with Implanted Deep Brain Stimulator
Jia Hui Wong1 and Ei Ei Nyein1
1Neuroradiology, National Neuroscience Institute Singapore, Singapore, Singapore
1Neuroradiology, National Neuroscience Institute Singapore, Singapore, Singapore
Synopsis
Magnetic Resonance Imaging (MRI) has been a widely used modality in patients with Deep Brain Stimulator (DBS) for a variety of neurological diseases. Radiofrequency heating still presents as a major concern in patient’s safety and exists as the most common limiting factor. This poster would help individuals to gain a deeper understanding about the importance of SAR considerations in patients with DBS whilst undergoing MRI without compromising patients safety and scan quality.
Background
Magnetic Resonance Imaging (MRI) has evolved into a fundamental tool used in patients with Deep Brain Stimulator (DBS) systems for electrode localization and to evaluate a wide range of disease processes. DBS systems have been approved as a surgical treatment in patients with conditions such as essential tremor, Parkinson’s disease (PD), Dystonia, Obsessive-compulsive disorder and Epilepsy [1]. Despite the advancements allowing most devices to become MRI compatible, safety concerns are still present with Radiofrequency (RF) heating being the most common limiting factor mentioned in literature to date. RF heating occurs in DBS patients, especially along conductive components built in the system. This is extremely detrimental as RF heating can cause a permanent neurological disorder. Hence safety considerations are to be implemented. Typical conditions that are considered clinically include the values of maximum specific absorption rate (SAR), gradient strengths as well as the type of RF coil used.Considerations
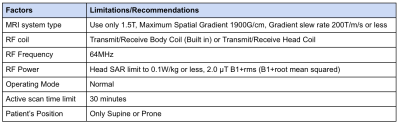
SAR is defined as the absorbed RF energy per unit of mass of an object, and is measured in watts per kilogram (W/kg)[2]. Generally, MRI scanners that are used in clinical settings derive an estimated SAR level for every scan; the factors that show in Table-1 are technical considerations according to the device manufacturer’s guidelines [3]. All these technical specifications and patient’s weight are taken into account before a scan; an estimated value of SAR is reflected on the scanning console. It is also known that SAR is proportional to the square of the magnitude of the electric field resulting in a higher concentration in the near-field region of the electrode. MRI induced electrode heating depends on a number of factors. This includes the placement of electrodes and extender wires, in which the total lead length and the nature of tissue would determine the overall heating concentration. In addition, depending on how iso-centre the IPG (Implantable Pulse Generator) is in the MR imaging unit and the type of coil used. These factors together with the chosen MR stimulation parameters would then dictate the energy deposition during imaging or SAR value [4][5]. According to the manufacturer's safety guidelines, routine clinical imaging can be performed at the lowest possible SAR/B1+rms.Conclusion
MRI as a modality contains exceeding diagnostic abilities in soft tissue differentiation and its immense anatomical detailing. It has grown to become a proposed prime modality used in patients with DBS. However, RF heating still exists as a major concern in patient’s safety to date. Hence, the above SAR considerations and technical considerations mentioned should be adhered throughout MRI scan without compromising on patient’s safety while acquiring a scan of diagnostic quality. Nevertheless, more extensive research is needed to provide a more comprehensive evaluation of heating not only just using SAR levels as a measure, where movement, induced current, and device functionality should also be studied.Acknowledgements
No acknowledgement found.References
1. National Neuroscience Institute (2017). Deep Brain Stimulation for Parkinson’s Disease. Available at: https://www.nni.com.sg/news/medical-news- singhealth/parkinson-disease-deep-brain-stimulation (Accessed: 20 September 2021).2. Baker, K.B., Tkach, J.A., Phillips, M.D. and Rezai, A.R., (2006). Variability in RF induced heating of a deep brain stimulation implant across MR systems. Journal of Magnetic Resonance Imaging: An Official Journal of the International Society for Magnetic Resonance in Medicine, 24(6), 1236-1242.
3. Medtronic. MRI guidelines for medtronic deep brain stimulation systems. Minneapolis, MN: Medtronic; 2015. (Accessed: 20 September 2021).
4. Mohsin, S. (2011). Concentration of the Specific Absorption Rate around Deep Brain Stimulation electrodes during MRI. Progress In Electromagnetics Research, 121, 469-484.
5. Franceschi, A. M., Wiggins, G. C., Mogilner, A. Y., Shepherd, T., Chung, S., & Lui, Y. W. (2016). Optimized, Minimal Specific Absorption Rate MRI for High-Resolution Imaging in Patients with Implanted Deep Brain Stimulation Electrodes. AJNR. American journal of neuroradiology, 37(11), 1996–2000.
DOI: https://doi.org/10.58530/2022/5053