5079
Evaluating Preparation Methods for Clinical MRI Scans in Young Children without Anesthesia1Alberta Children's Hospital, Calgary, AB, Canada
Synopsis
We compared the efficacy of three different preparation methods for clinical MRI scans without sedation in young children (3-7 years): at-home resources, a session with a child-life specialist, or a mock MRI session with a child life specialist. Success rates were excellent at 91%, with no differences between training groups. Subtle group differences in fear/anxiety ratings suggest a slight benefit of the mock MRI session in reducing anxiety before scans.
Background
The lack of ionizing radiation and ability to obtain high-resolution images of soft-tissue structures such as the heart and brain, make MRI a favourable choice for pediatric imaging.1 However, there is often difficulty, (or perceived difficulty) in obtaining useable MRI scans in young children due to motion and/or anxiety concerns.2 Young children (age <8 years at our study site) are typically scanned under general anesthetic (GA).3 GA permits the necessary MR images to be obtained without worry of movement, resulting in reliable high quality scans. However, GA introduces a small increased risk of side effects for the child,4,5 is costly, and presents logistical challenges for families and institutions.6 Further, there is ongoing concern about the potential impact of GA in early childhood on neurological development.7 There is a clear need for methods that allow children to undergo clinical MRI scans without GA. Previous work in both clinical and research settings has identified that preparation protocols, including the use of a mock MRI machine for training, may result in high success rates; however, there may be barriers to accessing this technology. We aimed to determine whether different preparation methods would enable young children to successfully undergo awake MRI scans.Methods
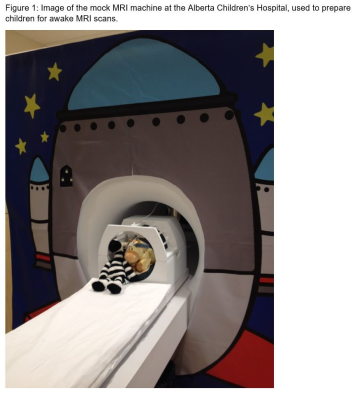
Children (3-7 years) scheduled for clinical MRI scans at the Alberta Children’s Hospital were invited to participate and randomly assigned to one of three groups: home-based preparation materials (including a book and recommended practice games), a session with a child life specialist (using toys, sound effects and other play-based materials but without a mock MRI scan), or a mock MRI session (Figure 1) with a child life specialist. Children underwent assigned training sessions a few days prior to their MRI scan. Self- and parent-reported anxiety were assessed pre and post-training (for the two training groups), and pre and post-MRI for all children. Scan success was determined by a radiologist and defined as obtaining images of high enough quality to answer the clinical question that prompted the MR scan. Children with unsuccessful scans were scheduled for another scan under GA.Results
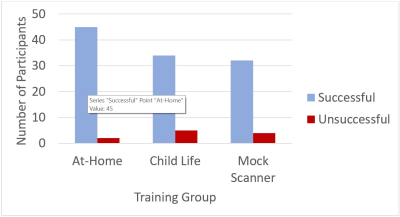
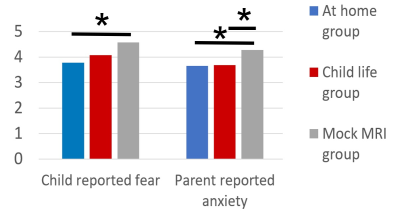
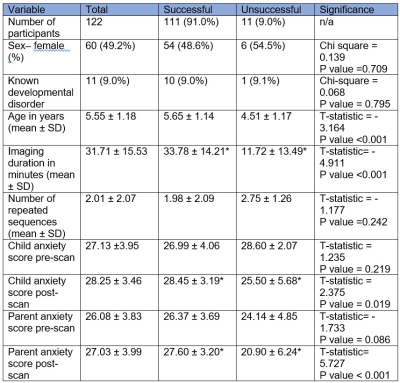
Overall success rate was 91% and did not differ significantly between training groups (Figure 2). Total anxiety scores were similar across groups both pre- and post-training (where applicable) and pre- and post-MRI scan. However, children in the mock MRI training group reported significantly lower fear (child self-report) and their parents reported less worry and feelings of being upset (parent-report; Figure 3) prior to the MRI scan. Children with unsuccessful scans were younger (4.5 vs. 5.7 years, p<0.001; Figure 4 and had significantly shorter scan durations that their successful counterparts (typically because scans were ended early). Parent-reported anxiety scores prior to the MRI scan were also significantly lower in children who were unsuccessful. Child life specialists and MRI technologists accurately predicted scan success (PPV 95.1% and 93.8% respectively).Conclusion
The high overall success rate suggests that young children can tolerate awake MRI scans and do not need to be routinely anesthetized. This would reduce the risks of side effects and the burden of anesthetized scans on the healthcare system and the family. All preparation methods tested, including at-home materials, seem efficacious in producing high success rates, with even most of the youngest children being successful. This suggests that minimally resource intensive preparations, delivered by the caregivers at home, could be implemented in areas where access to child-life specialists and/or mock MRI scanners may be limited. Group differences suggest that preparation with a mock MRI machine may reduce anxiety before MRI scanning, which could be beneficial especially for children undergoing multiple medical procedures.Acknowledgements
No acknowledgement found.References
1. Marshall SP, Smith MS, Weinberger E. Perceived anxiety of pediatric patients to magnetic resonance. Clin Pediatr (Phila). 1995;34(1):59–60.
2. Tyc V, Fairclough D, Fletcher B, Leigh L, Mulhern R. Children’s distress during magnetic resonance imaging procedures. J Child Heal Care. 1995;21(1):5–19.
3. Schulte-Uentrop L, Goepfert M. Anaesthesia or sedation for MRi in children. Curr Opin Anaesthesiol. 2010;23(4):513–7.
4. Slovis T. Sediation and anesthesia issues in pediatric imaging. Pediatr Radiol. 2011;41(Suppl 2):514.
5. Sanborn P, Michna E, Zurakowski D, Burrows P, Fontaine P, Connor L, et al. Adverse cardiovascular and respiratory events during sedation of pediatric patients for imaging examinations. Radiology. 2005;237(1):288–94.
6. Vanderby S, Babyn P, Carter M, Jewell S, McKeever P. Effect of anesthesia and sedation on pediatric MR imaging patient flow. Radiology. 2010;256(1):229–37.
7. Rappaport BA, Suresh S, Hertz S, Evers AS, Orser BA. Anesthetic neurotoxicity - clinical implications of animal models. N Engl J Med. 2015;372(9):796–7.
Figures