5077
3D Cranial Nerve Imaging with Background Suppression at 3T1Mermaid Beach Radiology, Gold Coast, Australia, 2Philips Healthcare ANZ Clinical Science, Sydney, Australia
Synopsis
Clinical presentations of many cranial nerve symptoms are scanned without an obvious gross pathology. The gold standard in MRI of high resolution multiplanar imaging with and without contrast often result in no obvious anatomical or post contrast injection enhancement changes. It involves a 3D fast spin echo Short Tau Inversion Recovery (STIR) with addition Motion Sensitive Driven Equilibrium (MSDE) preparation pulses for blood vessel/flow suppression. This sequence is improving our diagnostic confidence of cranial nerve neuropathies/neuritis with validation of perceived clinical indications.
Purpose
The purpose of this study is to design a sequence which can suppress vasculature and fat/background tissue to remove these challenges to help validate the clinical presentation, leading to increased confidence in diagnosis for validation of cranial nerve condition and immediate management of the patients. A significant number of presentations of cranial nerve symptoms are scanned without an obvious gross pathology. The gold standard in MRI of high resolution multiplanar imaging with and without contrast often result in no obvious anatomical or post contrast injection enhancement changes. This is often leads to either looking elsewhere for the source of the clinical presentation or a clinical decision that the pain is present due to a viral/medical condition and treat the patients’ symptoms based on anecdotally based clinically relevant information on top of the physical presentation. Examples of these include Bells palsy, trigeminal neuralgia and trochlea nerve related vision problems amongst other cranial conditions. There are challenges in this region such as multiple air/tissue interfaces causing local field inhomogeneities which are exacerbated at 3T, vasculature and the shape of anatomy which also help complicate and reduce sensitivity to subtle nerve related changes.Method
13 patients were scanned for cranial nerve related clinical indications including trigeminal neuralgia, diplopia and bells palsy. All scans were performed on a Philips Elition X 3T (Philips Netherlands). 3D Nerve view sequences were initially designed for brachial and lumbar plexus imaging for similar challenges. We redesigned this 3d sequence specifically for cranial nerves. It involves a 3D fast spin echo Short Tau Inversion Recovery (STIR) with addition Motion Sensitive Driven Equilibrium (MSDE) preparation pulses for blood vessel/flow suppression first described by Yoneyama et al (2). The RF pulses for both the MSDE and STIR Inversion pulses were modified for a significantly broader bandwidth for improved vessel suppression and fat/background suppression. The 3D flip angle modulation was changed to a tissue specific technique which enabled an adjustable plateau of transverse magnetisation coherence for short and medium T2 tissue species as well as the longer T2 tissues. This enables a short proton density weighted TE whilst using a significantly long echo train length creating a high signal to noise ratio, and a low TE which captures both short and long T2 nerve tissue species without blurring due to point spread function error. Using gadolinium-based contrast agent (GBCA) STIR pulse sequences leads to suppression of blood vessels and highly perfused tissues. Whilst this sequence can be used effectively without GBCAs, we routinely use it for neuropathy/neuritis-based protocols so using the sequence after the injection of contrast further enhances its ability to suppress very slow flowing veins as well as vascular tissue. Resolution was acquired at 0.9mm isotropic and interpolated to 0.45mm isotropic. Compressed SENSE (CS) was used to keep to a clinically viable scan time ~5-6 mins.Results
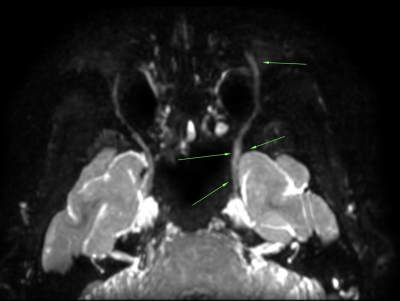
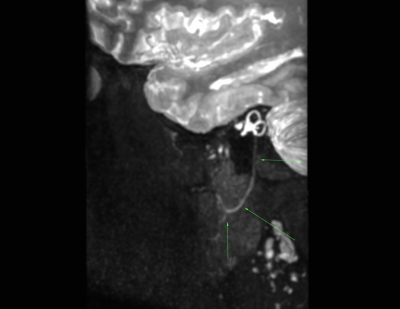
7 of the 13 patients with cranial nerve presentations demonstrated changes in the nerve sequence which were not noted by the Radiologist in routine imaging. They ranged from asymmetric visualisation (ie not normally seen unless inflamed), slight increase in diameter, increase in signal intensity or both. Validation was confirmed in patients with Trigeminal neuralgia (Figure 1) and trochlea (4th) nerve neuritis/palsy causing diplopia (Figure 2) and with facial nerve neuritis/Bells Palsy(Figure 3) One case could not use GBCA due to pregnancy for a Bells Palsy. Given less background suppression than we would normally see with GBCA, the effected facial nerve demonstrated asymmetric signal due to the fact that it usually can't be seen in the branches throughout the parotid gland and beyond. In cases involving the facial nerve and GBCAs, T13D black blood sequences also demonstrated contrast enhancement for further validation in another bells Palsy case.Discussion
This sequence is improveing our diagnostic confidence of cranial nerve neuropathies/neuritis with validation of perceived clinical indications. Using GBCAs is improving the sequence performance as it is used standardly in these protocols. Patients with changes received immediate treatment after there clinical presentations were validated with this imaging. Compressed SENSE was used to achieve clinically achievable scan times as well as de-noise the raw data for improved image quality. There has been other successful development of this sequence in its original form also with positive outcomes with non tissue specific pseudo steady state flip angle sweep which produces a longer TE (1). The main point of these modifications was to increase the proton density weighting whilst still maintaining a long echo train length without a blurring penalty and keep time efficiency. In previous comparison studies in the brachial plexus, we found this lower TE superior for SNR, and lesion conspicuity. There is still much to learn and optimise our TE and effective contrast to noise ratio further. Our next step in these cases is quantitative T2, T1 and T1rho mapping in the search for further quantitative validation.Acknowledgements
Mermaid Beach Radiology
Philips Healthcare Clinical Science Collaboration
Dr Iain Ball
Dr Zane Sherif
References
1.Cruyssen et al, 3D Cranial Nerve Imaging, a Novel MR Neurography Technique using Black Blood STIR TSE with a PSS Sweep and MSDE for visualisation of the Extraforaminal Cranial Nerve Branches, American Journal of Neuroradiology 2021, 42(3) 578-580, DOI:https://doi.org/10.3174/ajnr.A6904
2. Yoneyama et al, Rapid high resolution MR neurography with a diffusion weighted pre-pulse, Magn Reson Med Sci 2013;12:111-19, dot:10.2463/mrms.2012-0063 pmid23666153