5059
A conclusion on how computer-aided localization of a breast lesion impact Breast MRI-guided biopsies when compared with manual localization techniques1Radiology, Memorial Sloan Kettering Cancer Center, Forest Hills, NY, United States, 2Memorial Sloan Kettering Cancer Center, New York, NY, United States
Synopsis
Patients with suspicious lesions on MRI that cannot be detected with another modality may undergo MRI guided biopsy. The MRI biopsy may induce anxiety and may be uncomfortable with the breast in compression which may be exacerbated by the length of the procedure. Software has been developed by certain companies to streamline and increase ease of the MRI-guided biopsy. We performed a study to see if this software decreases the length of the procedure. We also will see if software leads to differences recommendation, concordance, and subsequent cancer if the biopsy was benign.
Background
Patients with suspicious lesions on MRI that cannot be detected with another modality may undergo MRI guided biopsy. The MRI biopsy may induce anxiety and may be uncomfortable with the breast in compression which may be exacerbated by the length of the procedure. Software has been developed by certain companies to streamline and increase ease of the MRI-guided biopsy. We performed a study to see if this software decreases the length of the procedure. We also will see if software leads to differences recommendation, concordance, and subsequent cancer if the biopsy was benign.Materials and Teaching Points
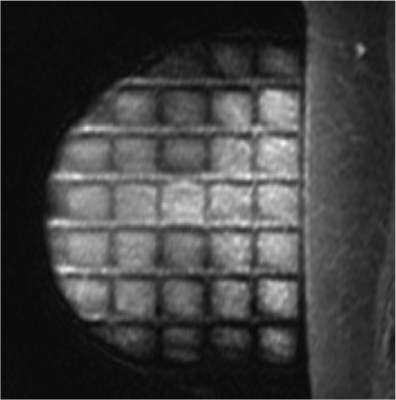
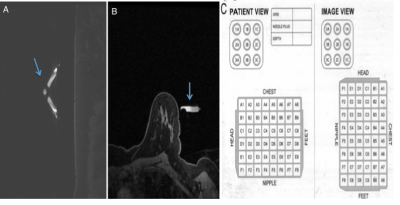
We conducted a retrospective review of patients from dates from December 2016 to December 2018 and included the first 100 consecutive patients to have undergone an MRI guided biopsy using software localizing approach and the first 99 consecutive patients to have undergone an MRI guided biopsy using a manual localizing approach. The software utilized by the institution was the Hologic software which requires a dedicated breast coil to successfully localized the target (Figure 1). MRI-guided biopsy with Manual Localization Technique When positioning the patient for breast biopsies one must ensure the require target is within the interventional grid to adequately cover the lesion of interest (Figure 2). The radiologist then evaluates compression and places a fiducial manually within the interventional grid to use as a reference for manual technique (figure 4). Manual Localization Technique: The protocol uses LAVA VIBRANT Flex for all sagittal views: slice thickness of 3mm; matrix size 256 x 192, field of view (FOV) 34-36, bandwidth of 200KHz, flip angle 10, The parameters for the second scan are axial scan with a slice thickness of 2mm and a FOV of 24-26. MRI-guided biopsy with Computer-aided software technique Follows the same principals as the manual technique. But one key measurement here is to ensure that the entirely of the fiducial is cover during the first diagnostic scan. If fiducial is not included computer registration will fail (Figure 5). Software Localization Technique: The protocol uses LAVA VIBRANT Flex for all sagittal views: slice thickness of 3mm; matrix size 256 x 192, field of view (FOV) 34-36, bandwidth of 200KHz, flip angle 10, The parameters for the second scan are axial scan with a slice thickness of 2mm and a FOV of 24-26Results
We compared the results between 100 patients who underwent an MRI-guided biopsy with software localizing approach and 99 patients who underwent an MRI-guided biopsy with manual localizing approach. There was no difference in size of target lesion, concordance of pathology results, follow up plan, malignant diagnosis, interval malignancy, and months of follow up between both groups. There were statistically more samples taken in the software group than the manual group (9.1 vs 8.3, p = 0.004). The procedure was statistically longer in manual group than the software group (33.0 minutes vs. 25.6 minutes, p = 0.0001) and the number of scans was more in the manual group than the software group (9.6 vs. 6.9, p = 0.0001).| Software | Manual | p | |
| Number of samples | 9.1 +/- 2.1 | 8.3 +/1 1.47 | 0.0041 |
| Procedure length, minutes | 25.6 +/- 7.9 | 33.0 +/- 16.1 | 0.0001 |
| Number of scans | 6.9 +/- 2.4 | 9.6 +/- 2.4 | 0.0001 |
| Mass/Focus (as opposed to Nonmass Enhancement) | 56.60% | 55% | 0.887 |
| Size, cm | 1.6 +/- 1.6 | 1.8 +/- 1.9 | 0.541 |
| Concordant pathology results | 98.00% | 99% | 0.621 |
| Definitive plan given (as opposed to 6-month f/u) | 83.8 | 85 | 0.847 |
| Malignancy Diagnosis | 17% | 19% | 0.716 |
| Follow up, months | 27.8 +/- 14.9 | 29.7 +/- 17.0 | 0.416 |
| Interval malignancy at time of follow up | 0% | 2% | 0.497 |
Conclusion
Software localizing approach in MRI-guided biopsy results in a shorter procedure and fewer scans which may help with the anxiety and discomfort of the patient. There is no difference in other outcome between when using software localizing approach versus manual localizing approach.Acknowledgements
No acknowledgement found.References
1. Boo-Kyung Han, Mitchell D. Schnall, Susan G. Orel, and Mark Rosen. Outcome of MRI-Guided Breast Biopsy. American Journal of Roentgenology 2008 191:6, 1798-1804
2. Chevrier M-C, David J, Khoury ME, Lalonde L, Labelle M, Trop I. Breast biopsies under magnetic resonance imaging guidance: challenges of an essential but imperfect technique. Curr Probl Diagn Radiol 2016;45(3):193-204.
3. Raza S, Chikarmane SA, Gombos EC, Georgian-Smith D, Frost EP. Optimizing Success and Avoiding Mishaps in the Most Difficult Image-guided Breast Biopsies. Seminars in Ultrasound, CT and MRI 2017;0(0).
4. 1. Morrison CK, Henze Bancroft LC, DeMartini WB, et al. Novel High Spatiotemporal Resolution Versus Standard-of-Care Dynamic Contrast-Enhanced Breast MRI: Comparison of Image Quality. Invest Radiol. 2017;52(4):198–205. doi:10.1097/RLI.0000000000000329