MRI as an Autopsy Tool & Its Use in the COVID Pandemic
1University of Sao Paulo - School of Medicine, Sao Paulo, Brazil
Synopsis
A medical imaging center (with US, CT and 7 Tesla MRI) integrated into the largest autopsy service for natural deaths in Latin America plays an important role in times of a pandemic. Recently, the SARS-CoV-2 pandemic has raised concerns around the world, requiring a rapid response combined with challenges due to biohazard. In this context, high-resolution MRI of the post mortem brain of deceased patients with COVID-19, with histological correlations, allows better understanding of COVID-19 beyond the characteristic primary pneumonia.
Brief
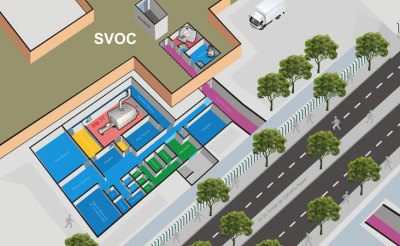
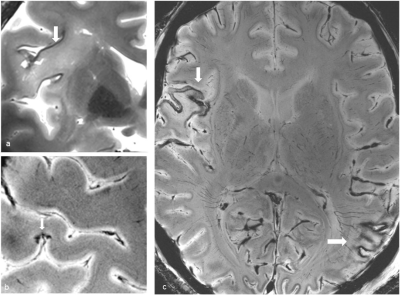
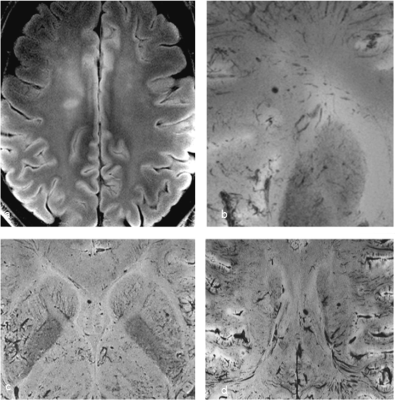
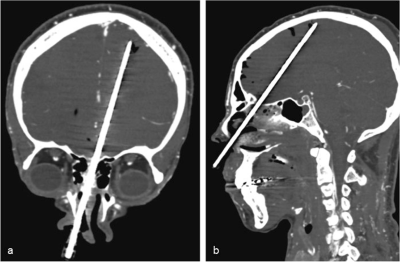
In Brazil, the law provides for the universal right to comprehensive health, as well as requiring a Death Certificate to bury a human body, which is provided by the government if families do not have a doctor. In the area of the city of São Paulo (about 20 million inhabitants) the Autopsy Service (SVOC) receives the majority of cases in which an autopsy is mandatory. Alone, SVOC performs over 13,000 autopsies/year, making it the largest autopsy service for patients who died of natural causes in the world. In addition, the SVOC and the central unit of the Forensic Doctor are located in the health quad where the Faculty of Medicine of the University of São Paulo (FMUSP) and the Public Clinical Hospital are located. FMUSP is the head of the largest health complex in Latin America. In this unique scenario, the Image Platform in the Autopsy Room (PISA) was created at FMUSP. PISA is part of the University of São Paulo's Multi-User Equipment Program, with direct route to the SVOC, and offers ultrasound, computed tomography and the first 7 Tesla full-body MRI machine in Latin America. This initiative aims to combine medical imaging and histological studies to better understand natural-death causes, including the development of minimally invasive autopsies (MIA). Prior to the SARS-CoV-2 pandemic, the previous yellow fever outbreak showed that ultrasound-based MIA has full diagnostic agreement with conventional autopsy. This approach allowed us to perform procedures on deceased COVID-19 patients at significantly lower risk compared to conventional autopsy. However, MRI-based MIA is the best approach to brain injury and was performed in some cases.The postmortem brain MRI was acquired in a 7T scanner with a 32-channel coil. Corpses were wrapped in appropriate plastic bags before entering the scanner. MRI protocols for post-mortem imaging need adaptation due to challenges that include: higher T1, shorter T2, higher magnetic susceptibility and lower ADC due to a combination of external factors like lower temperature and decomposition (that can be affected by post-mortem interval, ambient etc). After optimizations to fit with the time available for MRI procedures (around 1 hour), 3D-T1, coronal and axial T2, FLAIR, DWI and SWI images were acquired. A total body CT image was also acquired before MRI, and US-guided tissue sampling was performed after MRI. In summary, minimally invasive autopsy was an effective tool to assess underlying pathological brain changes in deceased COVID-19 patients, and MRI contributed to a better study of the brain, adding complementary information due to limitations of adult brain ultrasound and histology performed by biopsies.Acknowledgements
- Amaro Nunes Duarte‑Neto
- Claudia da Costa Leite
- Jair Theodoro Filho
- Maria da Graca Morais Martin
- Maria Concepcion Garcia Otaduy
- Marisa Dolhnikoff
- Liana Guerra Sanches
- Luiz Fernando Ferraz da Silva
- Paulo Hilario Nascimento Saldiva
- Renata Aparecida de Almeida Monteiro
References
Martin, M.d.G.M., Paes, V.R., Cardoso, E.F. et al. Postmortem brain 7T MRI with minimally invasive pathological correlation in deceased COVID-19 subjects. Insights Imaging 13, 7 (2022). https://doi.org/10.1186/s13244-021-01144-w
Dolhnikoff M, Ferreira Ferranti J, de Almeida Monteiro RA et al (2020) SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolescent Health 4:790–794. https://doi.org/10.1016/S2352-4642(20)30257-1
Duarte-Neto AN, Monteiro RAA, da Silva LFF et al (2020) Pulmonary and systemic involvement in COVID-19 patients assessed with ultrasound-guided minimally invasive autopsy. Histopathology 77:186–197. https://doi.org/10.1111/his.14160
Figures