Role of MR Imaging of Perianal Involvement in Pediatric & Adult Crohn Disease
1Beth Israel Deaconess Medical Center, Boston, MA, United States
Synopsis
Pelvic MRI is the standard of care in imaging perianal fistulae in patients with Crohn disease. Understanding the MR imaging protocol including scan planes and sequences used, is essential for accurate disease mapping. Knowledge of MR anatomy of the anal sphincter; types and classification of fistulae including complications and their imaging appearance at different stages of healing is of utmost importance for optimal patient care. This presentation will focus on the role of MRI in the diagnosis, various MR-classification systems used to describe perianal fistulizing disease, treatment response and prognostication of perianal Crohn disease in pediatric and adult patients.
Body
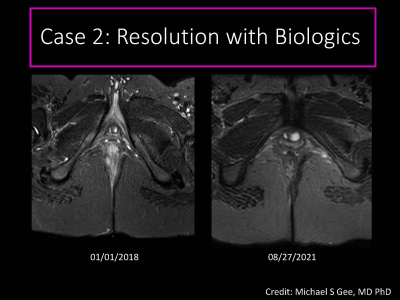
$$$Perianal involvement by fistulizing disease is a known debilitating manifestation of Crohn disease in adults and pediatric patients alike[1][2]. Besides surgical management, the course of this chronic disease has been altered by the introduction of biologic agents such as anti-tumor necrosis factor-alpha supplementing existing medical therapy[2]. This is turn, has necessitated accurate imaging diagnosis to help guide appropriate therapy and improve patient outcomes.$$$$$$MRI, with its absence of ionizing radiation, superior soft tissue resolution and multiplanar capability is the standard of care for imaging perianal fistulizing disease. Perianal MRI in the Crohn population is indicated in patients with any symptoms suggestive of perianal disease, detailed mapping of disease extent when partially imaged on MR enterography (MRE) or for ruling out an abscess that would prevent initiation of biologics.$$$
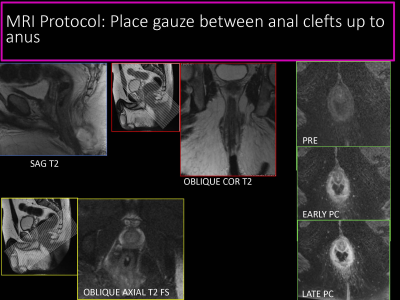
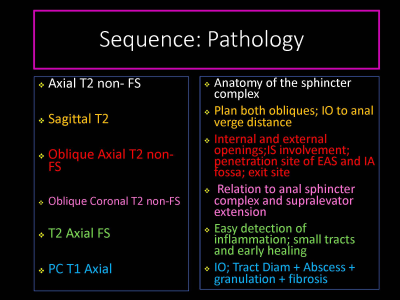
$$$At our institution, we offer a combined MR protocol, imaging both bowel and perianal region at the same time. Both pediatric and adult patients can be imaged supine on either a 1.5T or 3T machine using the same protocol and a phased array surface coil placed over the pelvis. No preparation is required prior to scanning. Protocols may vary slightly among various institutions, however, require a minimum of two planes perpendicular to each other. Following tri-plane localizer images, we obtain small field of view oblique axial and coronal T2-weighted sequences with and without fat suppression, using the longitudinal axis of the anal canal as the reference line, prescribed under supervision by radiologists’. Sagittal T2-weighted sequences and T1-weighted sequences in the oblique axial plane without and after administration of intravenous gadolinium-based contrast (0.1 mmol/kg) comprise a typical adult acquisition protocol [3]. A wide field of view pelvis is added to detect remote extensions of fistulas and assess bowel wall inflammation. Diffusion weighted images are often added to the pediatric protocol, especially if intravenous contrast cannot be administered[4]. The total scan time ranges from about 30 minutes for perianal MRI alone or an hour for a combined MRE and perianal MRI combination study.$$$
$$$Using a structured template report for interpretation assures standardization of terminology, decreased chance of missing key findings and potential for research[5]. The template used is often an institutional preference, however the ESGAR consensus guidelines appropriately illustrates all key elements to be described while interpreting these perianal MRI studies [6]. Traditionally, the surgical-based Parks Classification system and the MR basedSt. James University Hospital classification system have been used to describe fistulae, applicable in both pediatric and adult populations. However, these only provide anatomic localization without considering disease activity. The modified Van Assche index (mVAI) , an improvisation on the original MRI VAI proposed by the American Gastroenterology Association (AGA) in 2003 is an MR-based scoring system specific to the Crohn disease population, takes into account fistula inflammation in addition to anatomic localization [7][8]. The Magnetic Resonance Novel Index for Fistula Imaging in CD (MAGNIFI-CD) is an MRI based perianal inflammatory score demonstrating improved operating indices compared to mVAI, promising to be useful in clinical trials for assessment of treatment response, but needs additional validation [9]. The Pediatric MRI-based Perianal Crohn Disease (PEMPAC) Index is a recently described MRI based score exclusive to the pediatric population, enabling differentiation of the severity of disease activity and remission[10].$$$
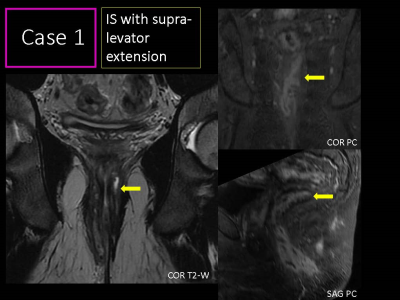
$$$A complete report would start by defining the fistula as simple or complex [11]. Thereafter, listing the number of fistulae, then focusing on each fistula individually to describe the internal anal opening based on the anal clock; course and traversing anatomic components of the anal sphincter complex and levator ani; external opening; single tract or presence of secondary tracts; associated sinus tracts or abscesses; extension to surrounding perineum; any post-surgical changes including presence of setons; disease activity based on MR signal characteristics and finally presence of rectal wall inflammation. As personalized medicine and advances in therapeutic options progress, newer imaging techniques are being explored to optimize patient care. 3D printed anal fistula models generated from high-resolution T2-weighted MRI volumetric data sets take about 6 hours to generate. These have been proposed to lower the inter-observer bias connected with interpretation of complex conventional MR imaging before planned surgery by Guz W et al [12]. Use of magnetization transfer imaging to create a standardized magnetization transfer ratio (MTR) parameter for predicting severity of intestinal fibrosis in Crohn disease patients is another example of newer advances [13][14].$$$
$$$Although progressive advancements in treatment have attempted to control and treat this debilitating condition, prognostic biomarkers are not yet robust in predicting treatment outcomes as also emphasized by Greer, Mary-Louise C and Taylor, Stuart A [4]. Since therapy relies heavily on accurate MR diagnosis, MRI can also play a complementary role as a prognostic biomarker [15][16][17]. More studies to prove MRI as a useful tool not only for initial diagnosis and surveillance but also to be used as a prognostic tool would indeed cement the role of MRI in imaging perianal Crohn disease in pediatric and adult patients. Finally, an opportunity to explore the role of MRI in Very Early Onset IBD (VEO-IBD) exists, with more research needed in this area. $$$
Acknowledgements
Sudha Anupindi, MD, FSAR; Attending Radiologist; Chief, Division of Body ImagingDirector, Section of Gastrointestinal and Hepatic Imaging; Soroosh Mahboubi Endowed Chair in Body ImagingAssociate Professor; Perelman School of Medicine at the University of Pennsylvania, PA.
Michael S Gee, MD, PhD; Attending Radiologist; Deputy Chair, Section Chief, Division of Pediatric Imaging, Massachusetts General Hospital for Children, Boston, MA.
References
1.Adler J, Dong S, Eder SJ, Dombkowski KJ (2017) Perianal Crohn Disease in a Large Multicenter Pediatric Collaborative. Journal of Pediatric Gastroenterology & Nutrition 64:e117–e124. https://doi.org/10.1097/MPG.00000000000014472.
2.Lopez N, Ramamoorthy S, Sandborn WJ (2019) Recent advances in the management of perianal fistulizing Crohn’s disease: lessons for the clinic. Expert Review of Gastroenterology & Hepatology 13:563–577. https://doi.org/10.1080/17474124.2019.16088183.
3.Santillan CS, Huang C, Eisenstein S, Al-Hawary MM (2021) MRI of Perianal Crohn Disease: Technique and Interpretation. Topics in Magnetic Resonance Imaging 30:63–76. https://doi.org/10.1097/RMR.00000000000002684.
4.Greer M-LC, Taylor SA (2021) Perianal Imaging in Crohn Disease: Current Status With a Focus on MRI, From the AJR Special Series on Imaging of Inflammation. American Journal of Roentgenology AJR.21.26615. https://doi.org/10.2214/AJR.21.266155.
5.Sudoł-Szopińska I, Santoro GA, Kołodziejczak M, et al (2021) Magnetic resonance imaging template to standardize reporting of anal fistulas. Tech Coloproctol 25:333–337. https://doi.org/10.1007/s10151-020-02384-66.
6.Halligan S, Tolan D, Amitai MM, et al (2020) ESGAR consensus statement on the imaging of fistula-in-ano and other causes of anal sepsis. Eur Radiol 30:4734–4740. https://doi.org/10.1007/s00330-020-06826-57.
7.van Rijn KL, Lansdorp CA, Tielbeek JAW, et al (2020) Evaluation of the modified Van Assche index for assessing response to anti-TNF therapy with MRI in perianal fistulizing Crohn’s disease. Clinical Imaging 59:179–187. https://doi.org/10.1016/j.clinimag.2019.10.0078.
8.Wang W-G, Lu W-Z, Yang C-M, et al (2020) Modified Van Assche magnetic resonance imaging-based score for assessing the clinical status of anal fistulas: Medicine 99:e20075. https://doi.org/10.1097/MD.00000000000200759.
9.Hindryckx P, Jairath V, Zou G, et al (2019) Development and Validation of a Magnetic Resonance Index for Assessing Fistulas in Patients With Crohn’s Disease. Gastroenterology 157:1233-1244.e5. https://doi.org/10.1053/j.gastro.2019.07.02710.
10.Choshen S, Turner D, Pratt L-T, et al (2021) Development and Validation of a Pediatric MRI-Based Perianal Crohn Disease (PEMPAC) Index—A Report from the ImageKids Study. Inflammatory Bowel Diseases izab147. https://doi.org/10.1093/ibd/izab14711.
11.Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB (2003) AGA technical review on perianal Crohn’s disease. Gastroenterology 125:1508–1530. https://doi.org/10.1016/j.gastro.2003.08.02512.
12.Guz W, Ożóg Ł, Aebisher D, Filip R (2021) The use of magnetic resonance imaging technique and 3D printing in order to develop a three-dimensional fistula model for patients with Crohn’s disease: personalised medicine. pg 16:83–88. https://doi.org/10.5114/pg.2020.10162913.
13.Pazahr S, Blume I, Frei P, et al (2013) Magnetization transfer for the assessment of bowel fibrosis in patients with Crohn’s disease: initial experience. Magn Reson Mater Phy 26:291–301. https://doi.org/10.1007/s10334-012-0355-214.
14.Meng J, Huang S, Sun C, et al (2020) Comparison of Three Magnetization Transfer Ratio Parameters for Assessment of Intestinal Fibrosis in Patients with Crohn’s Disease. Korean J Radiol 21:290. https://doi.org/10.3348/kjr.2019.021715.
15.Shenoy-Bhangle A, Nimkin K, Goldner D, et al (2014) MRI predictors of treatment response for perianal fistulizing Crohn disease in children and young adults. Pediatr Radiol 44:23–29. https://doi.org/10.1007/s00247-013-2771-516.
16.Karmiris K, Bielen D, Vanbeckevoort D, et al (2011) Long-Term Monitoring of Infliximab Therapy for Perianal Fistulizing Crohn’s Disease by Using Magnetic Resonance Imaging. Clinical Gastroenterology and Hepatology 9:130-136.e1. https://doi.org/10.1016/j.cgh.2010.10.02217.
17.Chambaz M, Verdalle-Cazes M, Desprez C, et al (2019) Deep remission on magnetic resonance imaging impacts outcomes of perianal fistulizing Crohn’s disease. Digestive and Liver Disease 51:358–363. https://doi.org/10.1016/j.dld.2018.12.010