Cardiac Relaxometry: Methods, Accuracy & Precision
Claudia Prieto1
1King's College London, London, United Kingdom
1King's College London, London, United Kingdom
Synopsis
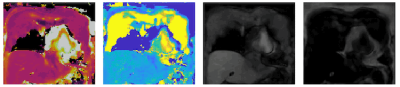
Myocardial tissue characterisation using T1, T2, and T2* mapping has emerged as a novel extremely useful clinical adjunct enabling detection of focal and diffuse fibrosis with T1 mapping, myocardial oedema with T2 mapping, extracellular volume with pre and post T1 mapping, iron overload with T2* mapping and fat fraction with a 3-point Dixon acquisition. This talk will introduce the basics of quantitative cardiac magnetic resonance imaging, focusing mainly on myocardial T1, T2 and T2* mapping.
Summary
Quantitative parameter mapping techniques have emerged to expand the diagnostic and prognostic value of cardiac MRI by promising quantitative characterisation and objective assessment of myocardial tissue properties. Several clinical studies have shown the potential of tissue specific parameters such as T1, T1rho, T2 and T2* relaxation times as well as extracellular volume (ECV) and fat fraction (FF) to improve the assessment of cardiovascular disease [1-10]. Native T1-mapping alone or in association with post-contrast T1-mapping for ECV quantification has been shown valuable for the assessment of a wide range of cardiac pathologies including acute and chronic myocardial infarction, myocarditis, cardiac amyloidosis, cardiac involvement in systemic disease and other cardiac conditions characterised by diffuse myocardial fibrosis [3]. T2* has an established role in the assessment and follow-up of iron overload cardiomyopathy [4]; and there is cumulating evidence of the importance of T2 mapping in detecting and quantifying myocardial edema in myocardial infarction, inflammatory cardiomyopathy or transplant heart rejection [5-6]. FF quantification has emerged as an important biomarker to characterise intramyocardial fat which is associated with poor prognosis and frequently results in severe heart failure [7-8]. More recently, T1rho mapping has shown promising results for the detection of focal and diffuse myocardial fibrosis without the need of exogenous contrast agents [9-10]. In this presentation, I will introduce the basics of quantitative cardiac relaxometry methods focusing mainly on myocardial T1, T2 and T2* mapping.Acknowledgements
The authors acknowledge financial support from the BHF PG/18/59/33955 and RG/20/1/34802, EPSRC EP/V044087/1, EP/P001009/, EP/P032311/1, EPSRC EP/P007619, Wellcome EPSRC Centre for Medical Engineering (NS/A000049/1), Fondecyt 1210637 & 1210638, Millennium Institute for Intelligent Healthcare Engineering iHEALTH ICN2021_004.References
- Messroghli DR, Moon JC, Ferreira VM, et al. Journal of Cardiovascular Magnetic Resonance 2017; 19:75 doi: 10.1186/s12968-017-0389-8.
- Ferreira VM, Schulz-Menger J, Holmvang G, et al. Journal of the American College of Cardiology 2018; 72:3158–3176 doi: 10.1016/j.jacc.2018.09.072.
- Haaf P, Garg P, Messroghli DR, Broadbent DA, Greenwood JP, Plein S. Journal of Cardiovascular Magnetic Resonance 2017; 18:89 doi: 10.1186/s12968-016-0308-4.
- Anderson L, Holden S, Davis B, et al. European Heart Journal 2001; 22:2171–2179 doi: 10.1053/euhj.2001.2822.
- Verhaert D, Thavendiranathan P, Giri S, et al. JACC: Cardiovascular Imaging 2011; 4:269–278 doi: 10.1016/j.jcmg.2010.09.023.
- Spieker M, Haberkorn S, Gastl M, et al. Journal of Cardiovascular Magnetic Resonance 2017; 19:38 doi: 10.1186/s12968-017-0350-x.
- Kellman P, Hernando D, Shah S, et al. Magnetic Resonance in Medicine 2009; 61:215–221 doi: 10.1002/mrm.21657.
- Mordi I, Radjenovic A, Stanton T, et al. JACC: Cardiovascular Imaging 2015; 8:1111–1112 doi: 10.1016/j.jcmg.2014.07.024.
- Witschey WRT, Zsido GA, Koomalsingh K, Kondo N, Minakawa M, Shuto T, McGarvey JR, Levack ML, Contijoch F, Pilla JJ, Gorman JH, Gorman RC. J Cardiovasc Magn Reson. 2012; 14:37.
- Han Y, Liimatainen T, Gorman RC, Witschey WR. Curr Cardiovasc Imaging Rep. 2014;7(2):9248.