Clinical Applications of 4D Flow MRI in the Portal Venous System
1Department of Radiology, University of Wisconsin-Madison, United States, 2Department of Radiology and Nuclear Medicine, Universität zu Lübeck, Lübeck, Germany
Synopsis
Assessment of hemodynamics in the portal venous system is essential for the diagnosis of many liver pathologies. 4D flow MRI offers a comprehensive approach for understanding pathophysiological mechanisms. It simultaneously and noninvasively acquires time-resolved flow and anatomic information in a 3D imaging volume. Although promising, it is particularly challenging in the portal venous system because of small vessel calibers, slow flow velocities, and respiratory motion. This presentation will describe how to perform and evaluate 4D flow MRI exams of the portal venous system. Moreover, it will discuss potential clinical applications and promising quantitative parameters that could help diagnose various pathologies.
Target Audience
Those with interest in clinical applications of 4D Flow MRI of the portal venous system including physicians and scientists.Learning Objectives
1. After this talk, the attendee will have basic knowledge on how to plan and analyze a 4D flow exam of the portal venous system.2. The attendee will be able to
- Identify potential clinical applications of 4D Flow MRI of the portal venous system.
- Give examples of relevant 4D Flow MRI parameters for pathologies in the portal venous system.
- Name remaining challenges for clinical implementation.
Introduction
Assessment of hemodynamics in the portal venous system is essential in the diagnosis of many liver pathologies. Alterations in portal venous flow and vascular morphology are often suggestive for disease1. Routinely used imaging modalities such as CT, ultrasound, invasive angiography, and MRI often focus on either capturing hemodynamics or morphology of the vessels. In contrast, 4D MRI offers a more comprehensive approach for the understanding of pathophysiological mechanisms by simultaneously and noninvasively acquiring time-resolved flow and anatomic information in a 3D imaging volume2. Although promising, 4D MRI in the portal venous system is particularly challenging because of small vessel calibers, slow flow velocities, and respiratory motion3.Purpose
This presentation will describe how to perform and evaluate 4D MRI examinations of the portal venous system. Moreover, it will discuss potential clinical applications and promising quantitative parameters that could help to diagnose various pathologies.Acquisition of 4D Flow MRI in the Portal Venous System
4D flow MRI of the portal venous system can be acquired with or without contrast agent at both 1.5T or 3.0T2, 3. Most MRI vendors offer 4D flow MRI as a product sequence. When considering whether to optimize spatial or temporal resolution for a given acquisition time, the emphasis should be on high spatial resolution to resolve the relatively small vessels of interest. Temporal resolution is of secondary importance because of the relatively constant flow in the portal vein4. Respiratory gating is critical to reduce motion artifacts. For portal venous imaging, a typical velocity encoding setting (venc) is 60cm/s. If higher velocities are expected, e.g., for imaging after transjugular intrahepatic portosystemic shunt (TIPS), a higher venc of 80-120cm/s may be helpful5.Patients should be fasting for 5 hours prior to the MR exam to exclude postprandial hyperemia of the gastrointestinal tract which could prohibit comparison to reference values6.
Post Processing, Quality Control, and Analysis
Post processing of 4D flow MRI should include correction for concomitant gradient field effects (Maxwell terms), phase background effects due to eddy currents2, and phase unwrapping in the presence of velocity aliasing7. Quality assurance should include 1) visual inspection of magnitude and phase contrast datasets, and 2) conservation of mass analysis to confirm coherent measurements (e.g., flow volume in portal vein should be equal to flow volume in right and left portal vein), Fig. 1. Several software tools are available for the analysis of 4D flow MRI data, ranging from internally developed solutions to regulatory-approved software packages for purchase. Typical analysis parameters of a vessel cross-section include velocity (cm/s) and flow rate (L/min). Pathline and streamline analysis helps identify regions of reversed flow and focal acceleration. Time-averaged complex difference angiograms allow anatomic assessment of the portal vasculature, especially the detection of anatomic variants and varices.Potential Clinical Applications
Diagnosis and risk stratification of liver cirrhosis and portal hypertension:Cirrhosis is characterized by advanced liver fibrosis, liver failure and portal hypertension. Patients with portal hypertension can develop portosystemic collaterals that shunt blood away from the liver8 (Fig. 2). The most clinically relevant collaterals are gastroesophageal varices that are fragile and can rupture easily, often leading to life-threatening bleeding8. Currently, invasive pressure measurements and recurrent esophagogastroduodenoscopy (EGD) examinations are routinely used for diagnosis and follow-up of portal hypertension9-11.
Early studies have shown very promising results indicating that 4D flow MRI may be suitable for the non-invasive identification of high-risk gastroesophageal varices: Motosugi et al12 focused on two characteristic hemodynamic changes to identify patients with high-risk varices: 1) flow reversal in the left gastric vein indicating shunting towards gastroesophageal varices and 2) increased flow in the azygos vein indicating increased drainage of gastroesophageal varices into the systemic circulation (Fig. 3).
Roldán-Alzate et al6 proposed another promising approach to diagnose and grade liver cirrhosis. They analyzed portal venous hemodynamics after fasting as well as after a standardized meal challenge.
After a meal challenge, flow volumes in portal vein and superior mesenteric vein increased to a lesser extent in patients as compared to healthy volunteers. Moreover, they found a significant increase in azygos vein blood flow in patients with cirrhosis after the meal challenge, indicating increased portosystemic shunting volume.
Multiple studies reported flow reversal in the portal vein, superior mesenteric vein, or splenic vein, as well as direct visualization and measurement of collateral flow, e.g., in the umbilical vein, in some patients with advanced cirrhosis6, 12-16.
Surgical planning and follow-up of transjugular intrahepatic portosystemic shunts (TIPS):
Patients with portal hypertension that cannot be controlled by drug therapy can be treated by creating a portosystemic venous shunt that diverts flow from the portal venous system directly into the systemic circulation, bypassing the liver. 4D flow MRI can confirm a significant increase in flow volume and peak velocity in the portal venous system after the procedure. Moreover, it allows the measurement of the shunt fraction, i.e., flow volume in the shunt in relation to the portal vein5, 17-19. It is also a valuable diagnostic tool to evaluate possible shunt dysfunction by identifying increased velocity in a stenosis19 or previously unknown arterio-portal-venous shunts5.
Surgical planning and follow-up of liver transplantation:
Initial studies suggest that pre-operative 4D flow MRI of the portal venous system can be used for surgical planning and prediction of post-surgical outcome in donors and recipients of living liver transplants20. At some sites, post-operative 4D flow MRI already helps inform treatment decisions21, 22.
Remaining Challenges for Clinical Implementation
As we move toward clinical application, large multicenter, multi-vendor follow-up studies are needed to confirm the diagnostic value of 4D flow MRI in the portal venous system. In addition, workflow improvements, including standardized and faster acquisition and post-processing, will facilitate broad clinical application.Conclusion
4D flow MRI can improve the understanding and diagnosis of clinically relevant pathologies of the portal venous system by providing temporally resolved information on hemodynamics and morphology of the respective vessels. One of the most promising clinical applications is the diagnosis and risk stratification of cirrhotic liver disease.Acknowledgements
Dr. Oechtering receives funding from the German Research Foundation (OE 746/1-1). GE Healthcare provides research support to the University of Wisconsin.
References
1. Mcnaughton DA and Abu-Yousef MM. Doppler US of the Liver Made Simple. RadioGraphics. 2011;31(1):161-188
2. Dyverfeldt P, Bissell M, Barker AJ, Bolger AF, Carlhall CJ, Ebbers T et al. 4D flow cardiovascular magnetic resonance consensus statement. J Cardiovasc Magn Reson. 2015;17(1):72.
3. Oechtering TH, Roberts GS, Panagiotopoulos N, Wieben O, Reeder SB, and Roldán-Alzate A. Clinical Applications of 4D Flow MRI in the Portal Venous System. Magnetic Resonance in Medical Sciences. 2022.
4. Landgraf BR, Johnson KM, Roldan-Alzate A, Francois CJ, Wieben O, and Reeder SB. Effect of temporal resolution on 4D flow MRI in the portal circulation. J Magn Reson Imaging. 2014;39(4):819-26.
5. Bannas P, Roldan-Alzate A, Johnson KM, Woods MA, Ozkan O, Motosugi U et al. Longitudinal Monitoring of Hepatic Blood Flow before and after TIPS by Using 4D-Flow MR Imaging. Radiology. 2016;281(2):574-582.
6. Roldan-Alzate A, Frydrychowicz A, Said A, Johnson KM, Francois CJ, Wieben O et al. Impaired regulation of portal venous flow in response to a meal challenge as quantified by 4D flow MRI. J Magn Reson Imaging. 2015;42(4):1009-17.
7. Loecher M, Schrauben E, Johnson KM, and Wieben O. Phase unwrapping in 4D MR flow with a 4D single-step laplacian algorithm. J Magn Reson Imaging. 2016;43(4):833-42.
8. Garcia-Tsao G, Groszmann RJ, Fisher RL, Conn HO, Atterbury CE, and Glickman M. Portal pressure, presence of gastroesophageal varices and variceal bleeding. Hepatology. 1985;5(3):419-24.
9. De Franchis R. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53(4):762-8.
10. Garcia-Tsao G, Abraldes JG, Berzigotti A, and Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65(1):310-335.
11. Garcia-Tsao G, Sanyal AJ, Grace ND, and Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-38.
12. Motosugi U, Roldan-Alzate A, Bannas P, Said A, Kelly S, Zea R et al. Four-dimensional Flow MRI as a Marker for Risk Stratification of Gastroesophageal Varices in Patients with Liver Cirrhosis. Radiology. 2019;290(1):101-107.
13. Stankovic Z, Csatari Z, Deibert P, Euringer W, Blanke P, Kreisel W et al. Normal and altered three-dimensional portal venous hemodynamics in patients with liver cirrhosis. Radiology. 2012;262(3):862-73.
14. Stankovic Z, Frydrychowicz A, Csatari Z, Panther E, Deibert P, Euringer W et al. MR-based visualization and quantification of three-dimensional flow characteristics in the portal venous system. J Magn Reson Imaging. 2010;32(2):466-75.
15. Roldan-Alzate A, Francois CJ, Wieben O, and Reeder SB. Emerging Applications of Abdominal 4D Flow MRI. AJR Am J Roentgenol. 2016;207(1):58-66.
16. Roldan-Alzate A, Frydrychowicz A, Niespodzany E, Landgraf BR, Johnson KM, Wieben O et al. In vivo validation of 4D flow MRI for assessing the hemodynamics of portal hypertension. J Magn Reson Imaging. 2013;37(5):1100-8.
17. Stankovic Z, Blanke P, and Markl M. Usefulness of 4D MRI flow imaging to control TIPS function. Am J Gastroenterol. 2012;107(2):327-8.
18. Stankovic Z, Rossle M, Euringer W, Schultheiss M, Salem R, Barker A et al. Effect of TIPS placement on portal and splanchnic arterial blood flow in 4-dimensional flow MRI. Eur Radiol. 2015;25(9):2634-40.
19. Owen JW, Saad NE, Foster G, and Fowler KJ. The Feasibility of Using Volumetric Phase-Contrast MR Imaging (4D Flow) to Assess for Transjugular Intrahepatic Portosystemic Shunt Dysfunction. J Vasc Interv Radiol. 2018;29(12):1717-1724.
20. Rutkowski DR, Reeder SB, Fernandez LA, and Roldan-Alzate A. Surgical planning for living donor liver transplant using 4D flow MRI, computational fluid dynamics and in vitro experiments. Comput Methods Biomech Biomed Eng Imaging Vis. 2018;6(5):545-555.
21. Lenz A, Fischer L, Li J, and Bannas P. 4D Flow MRI for Monitoring Portal Flow in a Liver Transplant Recipient with a Renoportal Anastomosis. Rofo. 2019;191(9):847-848.
22. Hyodo R, Takehara Y, Mizuno T, Ichikawa K, Ogura Y, and Naganawa S. Portal Vein Stenosis Following Liver Transplantation Hemodynamically Assessed with 4D-flow MRI before and after Portal Vein Stenting. Magn Reson Med Sci. 2020.
Figures
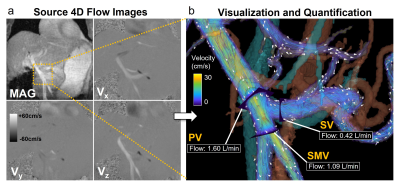
Fig. 1: a) Quality analysis includes inspection of velocity images (Vx, Vy, Vz) and magnitude (MAG) images. b) In a second step, flow measurements in the superior mesenteric vein (SMV) and the splenic vein (SV) should approximately add up to the flow volume of the portal vein. Velocity information is visualized by color-coded streamlines with white arrows depicting the direction of blood flow in the portal venous system. Adapted after Oechtering TH et al, MRMS, 2022.
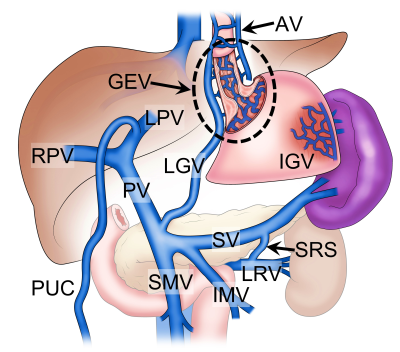
Fig. 2: Schematics of portosystemic collaterals in portal hypertension: Gastroesophageal varices (GEV) fed by reversed flow in the left gastric vein (LGV) and draining into the azygos vein (AV), paraumbilical collaterals (PUC) from the left portal vein (LPV), isolated gastric varices (IGV) from the splenic circulation, and spontaneous splenorenal shunt (SRS) with flow from the splenic vein (SV) into the left renal vein (LRV). IMV = inferior mesenteric vein, PV = portal vein, RPV = right portal vein, SMV = superior mesenteric vein. Adapted after Oechtering TH et al, MRMS, 2022.
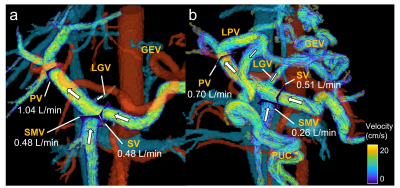
Fig. 3: Risk assessment of gastroesophageal varices (GEV). White arrows and streamlines indicate flow direction. (a) 64-year-old male with endoscopically confirmed varices at low risk of bleeding. Note the hepatopetal flow (= towards the liver) in the left gastric vein (LGV), superior mesenteric vein (SMV), splenic vein (SV), and portal vein (PV). (b) 54-year-old male with high-risk varices and hepatofugal flow (= away from the liver) in the LGV and GEV. This patient also has paraumbilical collaterals (PUC) supplied by the left portal vein (LPV). after Oechtering TH et al, MRMS, 2022.