4961
Parameters associated with durable clinical success in a multi-center trial using MR guided focused ultrasound treat uterine leiomyomas1Radiology, Stanford University, Stanford, CA, United States, 2Allegheny Health Network, Pittsburgh, PA, United States, 3Radiology, Mayo Clinic, Rochester, MN, United States, 4Radiology, UCLA, Los Angeles, CA, United States, 5Radiology and Medical Imaging, University of Virginia, Charlottesville, VA, United States, 6Interventional Radiology, Ohio Health, Columbus, OH, United States, 7Radiology, UCSF, San Francisco, CA, United States, 8Obstetrics and Gynecology, Duke University, Durham, NC, United States, 9Radiology, Brigham and Women's Hospital, Boston, MA, United States
Synopsis
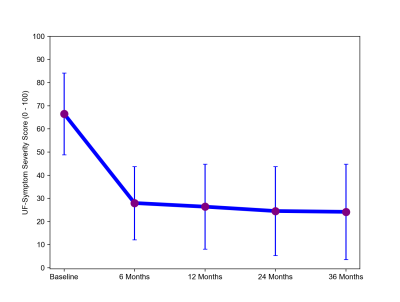
This study presents results of a prospective multicenter clinical trial of 99 women treated with MR guided focused ultrasound (MRgFUS) for symptomatic uterine leiomyomas to assess treatment durability and to evaluate potential demographic, imaging, and technical characteristics associated with lasting clinical outcomes. Following treatment, there was an improvement in symptoms, with a significant decrease in mean symptom severity score at the 6, 12, 24 and 36 month follow up (p<0.001). In a multivariate model, a new parameter of interest, the ratio of non-perfused volume to total fibroid volume (NPV/TFV) was found to be predictive of durable clinical success (p=0.03).
Introduction
Since the introduction of MR guided focused ultrasound (MRgFUS), single center studies have described improved outcomes after technological advances and evolution of screening and treatment approaches to overcome some early limitations and to target high ablation volumes (1–3). This study presents results of a multicenter clinical trial, incorporating these technical and treatment advances, to assess treatment durability of MRgFUS for symptomatic uterine fibroids, and to evaluate what characteristics are associated with lasting clinical outcomes.Methods
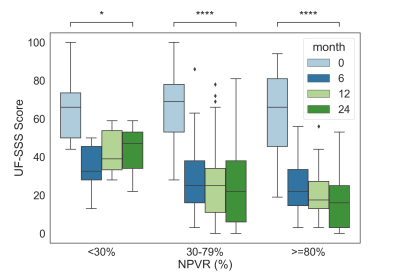
A prospective, multi-center clinical trial was conducted of 99 women treated with MRgFUS for uterine fibroids across 8 clinical sites. Patient follow up was conducted at 6 month, 12 month, 24 month, and 36 month time point using the Uterine Fibroid Symptom (UF) questionnaire. Patient demographics, imaging characteristics (such as T2 intensity compared with surrounding myometrium, Funaki classification), and treatment-related parameters associated with durable clinical outcomes were analyzed using both univariate and multivariate logistic regression models. Patients who experienced a 30% or greater reduction of symptom severity score (SSS) on the UF were considered responders. Durable clinical success was defined as those patients who were responders at both the 12 and 24 month time points. The 36 month time point was excluded from logistic model to preserve statistical power (patients lost to follow-up). Immediate post treatment contrast enhanced non-perfused volume to target fibroid volume ratio (NPVR) was categorized into three ablation success subgroups, NPVR = <30%, 30 – 79%, and >=80% and compared with outcomes at follow up time points.Results
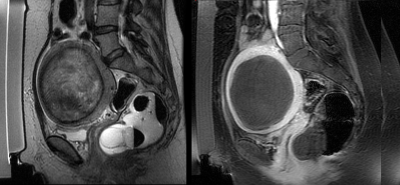
Figure 1 shows an example of a 41 year-old woman with a 570 cc fibroid tumor treated with MRgFUS, immediate post contrast T1 weighted images show a 99% NPVR was achieved. Following treatment, there was an improvement in symptoms, with a significant decrease in mean SSS at the 6, 12, 24 and 36 month follow up (p < 0.001 for all time points) (Figure 2). Of the entire treatment cohort, 12 patients (12%) ultimately went on to have an alternative treatment, including hysterectomy (n=6) and myomectomy (n=6). In univariate analysis, 3 variables predicted sustained clinical treatment success at both the 12 month and 24 month time points: NPVR (p = 0.02), absence of T2 Funaki Type 2 (p = 0.02), and the ratio of non-perfused volume to total fibroid volume (NPV/TFV) (p = 0.002). Neither the location of the fibroid, nor technical variables such as sonication energy (p = 0.48) or maximum temperature (p = 0.33) were stand-alone predictors of durable clinical success. In the multivariate model, the ratio of non-perfused volume to total fibroid volume (NPV/TFV) was found to be predictive of durable clinical success (p = 0.03). An NPV/TFV at least 40% resulted in clinical success in 83% of the patients. Although NPVR was not a strong predictor in the multivariate model, patients with an NPV ratio below 30% had less improvement from baseline, and significantly different UF SSS scores at 24 months than those with higher NPV ratios (30% vs. 30-79%, p = 0.05, 30% vs 80%, p = 0.01) (Figure 3).Discussion/Conclusion
While NPVR has typically been the primary predictor of patient outcome, a recent comprehensive meta-analysis surprisingly did not show an association between NPVR and symptom relief(4–6). This study may explain this discrepancy by revealing a new parameter of interest, the ratio of NPV to the uterine total fibroid volume (TFV), as the parameter which predicts durable clinical response, maintained at both the 12 and 24 month time points. This finding is useful to identify patients who would benefit most from MRgFUS by taking into account not only previously reported factors such as their T2 Funaki status, subcutaneous fat thickness, and fibroid perfusion, but also the total fibroid volume, including the volume of other fibroids which can contribute to the durability of clinical success.Acknowledgements
Authors would like to thank Jarrett Rosenberg for meaningful discussion.References
References:
1. Trumm CG, Stahl R, Clevert D-A, et al. Magnetic resonance imaging-guided focused ultrasound treatment of symptomatic uterine fibroids: impact of technology advancement on ablation volumes in 115 patients. Invest Radiol 2013;48:359–365.
2. Keserci B, Duc NM. Magnetic Resonance Imaging Parameters in Predicting the Treatment Outcome of High-intensity Focused Ultrasound Ablation of Uterine Fibroids With an Immediate Nonperfused Volume Ratio of at Least 90. Acad Radiol 2018;25:1257–1269.
3. Verpalen IM, de Boer JP, Linstra M, et al. The Focused Ultrasound Myoma Outcome Study (FUMOS); a retrospective cohort study on long-term outcomes of MR-HIFU therapy. Eur Radiol 2020;30:2473–2482.
4. Mindjuk I, Trumm CG, Herzog P, Stahl R, Matzko M. MRI predictors of clinical success in MR-guided focused ultrasound (MRgFUS) treatments of uterine fibroids: results from a single centre. Eur Radiol 2015;25:1317–1328.
5. Gorny KR, Woodrum DA, Brown DL, et al. Magnetic Resonance–guided Focused Ultrasound of Uterine Leiomyomas: Review of a 12-month Outcome of 130 Clinical Patients. Journal of Vascular and Interventional Radiology 2011;22:857–864.
6. Verpalen IM, Anneveldt KJ, Nijholt IM, et al. Magnetic resonance-high intensity focused ultrasound (MR-HIFU) therapy of symptomatic uterine fibroids with unrestrictive treatment protocols: A systematic review and meta-analysis. European Journal of Radiology 2019;120:108700.
Figures