4950
3T Chemical Shift encoded MRI detects Bone Marrow Adipose Tissue changes In Osteoporosis with Fragility Fracture
Dimitri Martel1, Benjamin Leporq2, Anmol Monga1, Stephen Honig3, and Gregory Chang1
1Radiology, NYU Langone Health, New York, NY, United States, 2Université de Lyon; CREATIS CNRS UMR 5220, Inserm U1206, INSA-Lyon, Villeurbanne, France, 3Osteoporosis Center, Hospital for Joint Diseases, NYU Langone Health, New York, NY, United States
1Radiology, NYU Langone Health, New York, NY, United States, 2Université de Lyon; CREATIS CNRS UMR 5220, Inserm U1206, INSA-Lyon, Villeurbanne, France, 3Osteoporosis Center, Hospital for Joint Diseases, NYU Langone Health, New York, NY, United States
Synopsis
Osteoporosis (OP) is associated with low bone mass and deterioration of bone tissue microarchitecture leading to increased bone fragility and fracture risk. There are increasing pieces of evidence that bone marrow adipose tissues (BMAT) play a significant role in the pathophysiology of osteoporosis. Our aim was to assess the proximal femur BMAT composition in OP without (OP) and with history of fragility fracture (OP-Fx) and compare it to naive controls using Chemical Shift Encoded MRI.
Introduction
Osteoporosis (OP) is associated with low bone mass and deterioration of bone tissue microarchitecture leading to increased bone fragility and fracture risk, especially in the proximal femur. OP is a serious public health concern, with an estimated over 200 million people worldwide suffering from this disease(1). Current standard-of-care methods to assess OP and fracture risk include Dual-Energy X-ray absorptiometry (DXA). DXA is relatively easy to perform in the clinic, and the amount of radiation exposure is considered low. However, it is limited by its low sensitivity, as the majority of patients with increased fracture risk do not have osteoporotic BMD. There are increasing pieces of evidence that bone marrow adipose tissues (BMAT) play a significant role in the pathophysiology of osteoporosis(2,3). Using magnetic resonance spectroscopy, an increased quantity of total fat and decreased quantity of unsaturated fatty acids in BMAT has been observed in the proximal femur of OP subjects compared to controls, and increased total BMAT has been observed in the vertebrae of subjects with OP(4,5). In addition, BMAT composition has been linked with fragility fractures and diabetes in the vertebrae(6). In more recent work, it has been found subregional differences in the femur in terms of poly and mono unsaturation in BMAT between primary and secondary osteoporosis in the more biomechanical stressed subregions of the proximal femur suggesting a lipotoxic role of BMAT in OP progression and in bone quality using a Chemical Shift Encoded MRI method(7).Our aim was to assess the proximal femur BMAT composition in OP without (OP) and with history of fragility fracture (OP-Fx) and compare it to naive controls.Material/Method
This study had institutional review board approval and written informed consent was obtained from all subjects. All subjects were recruited from the Rheumatology division at our institution.The subject characteristics are provided in table 1. MR acquisitions were performed on a 3T system (Siemens healthcare, Erlangen, Germany) using an 3D spoiled gradient echo sequence with a n=12 echoes train length (n ×1.2ms) with flyblack readout gradient. TR/FA = 16ms/5° and BW= 2000 Hz/px. 32 coronal slices were acquired. Using method described in (8) , fat content (i.e. Proton Density Fat Fraction (PDFF)) and fatty acid composition quantification (i.e. saturated (SFA), monounsaturated (MUFA) and polyunsaturated (PUFA)) were computed as parametric maps. Subregions of the proximal femur were defined by drawing ROIs in the femoral head, femoral neck, trochanter area and femoral shaft. Statistical differences were investigated through Kruskal-Wallis non-parametric test with null hypothesis that the median value of each index across the three groups are equal and a statistical threshold of p < 0.05 to reject the null hypothesis.Results
Typical parametric maps are shown in Figure 1. Difference between groups are shown in Figure 2. No differences were found in term of PDFF. In term of fatty acids composition and compared to controls and OP: OP-Fx show lower SFA in trochanter (respectively -9.3% and-5.4%, p<0.05), higher MUFA in the whole femur (respectively +5.1% and 5.5%) and higher PUFA in femoral neck (+3.2% and 2.9%, p<0.05). Also, in femoral head OP-Fx has higher MUFA compared to controls (+7.1%, p<0.05) and higher PUFA (+3.6%, p<0.01); in femoral neck OP-Fx has lower SFA compare to OP (-8.6%, p<0.05). For OP, differences with controls were found in femoral neck (MUFA: +8.6%, PUFA: +2.9%).Discussion/Conclusion
Fatty acids composition in femur exhibits a higher level of unsaturated fatty acids in OP subjects. In particular, OP-Fx show higher MUFA levels in femur and higher PUFA in femoral head and neck suggesting a specific lipid profile for fragility fracture history in femur. These results provide further evidence for the role of marrow fat composition in bone health.Acknowledgements
No acknowledgement found.References
1. Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 1993;94(6):646-650.2. Cawthorn WP, Scheller EL, Parlee SD. Expansion of Bone Marrow Adipose Tissue During Caloric Restriction Is Associated With Increased Circulating Glucocorticoids and Not With Hypoleptinemia. Endocrinology 2015;157:508-521.
3. Scheller EL, Doucette CR, Learman BS, et al. Region-specific variation in the properties of skeletal adipocytes reveals regulated and constitutive marrow adipose tissues. Nat Commun 2015;6:7808.
4. Griffith JF, Guglielmi G. Bone Marrow Changes in Osteoporosis. In Osteoporos Bone Densitom Meas Edited by Berlin Heidelberg Springer Berlin Heidelberg;2013 SRC - GoogleScholar:69-85.
5. Yeung DKW, Griffith JF, Antonio GE, Lee FKH, Woo J, Leung PC. Osteoporosis is associated with increased marrow fat content and decreased marrow fat unsaturation: A proton MR spectroscopy study. J Magn Reson Imaging 2005;22(2):279-285.
6. Patsch JM, Li X, Baum T, et al. Bone marrow fat composition as a novel imaging biomarker in postmenopausal women with prevalent fragility fractures. J Bone Miner Res 2013;28(8):1721-1728.
7. Martel D, Leporq B, Bruno M, Regatte RR, Honig S, Chang G. Chemical shift-encoded MRI for assessment of bone marrow adipose tissue fat composition: Pilot study in premenopausal versus postmenopausal women. Magn Reson Imaging 2018;53:148-155.
8. Martel D, Leporq B, Saxena A, et al. 3T chemical shift‐encoded MRI: Detection of altered proximal femur marrow adipose tissue composition in glucocorticoid users and validation with magnetic resonance spectroscopy. J Magn Reson Imaging 2019;50(2):490-496.
Figures
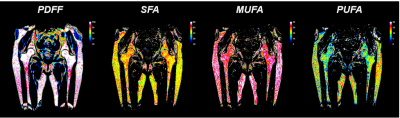
Figure 1: Typical reconstructed parametric maps (PDFF: proton density fat fraction, MUFA: mono-unsaturated fat, PUFA: poly-unsaturated fat, SFA: saturated fat)
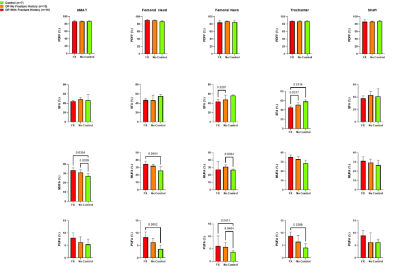
Figure 2: Boxplot of integrated parametric values in each subregions for Fx (osteoporosis subjects with fragility fracture history), No (osteoporosis subjects without fragility fracture history) and controls.
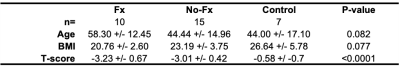
Table 1: Subjects and groups demographics
DOI: https://doi.org/10.58530/2022/4950