4932
Evaluating the clinical significance of MRI findings of Brain Herniations into Arachnoid Granulations in patients with pulsatile tinnitus1Radiology, UCSF, San Francisco, CA, United States, 2Radiology, University of Wisconsin, Madison, WI, United States, 3Neurology, UCSF, San Francisco, CA, United States
Synopsis
Pulsatile tinnitus, a severely debilitating condition where a “whooshing” sound is heard with each heart beat, affects over 3 million Americans, leading to anxiety, depression and even suicide. While many there are many diseases associated with pulsatile tinnitus one common and serious condition is idiopathic intracranial hypertension. Our study is the first to show that the presence of brain herniations through arachnoid granulations into dural sinuses on MRI is significantly associated with idiopathic intracranial hypertension in patient's with pulsatile tinnitus.
Introduction
Pulsatile tinnitus, a severely debilitating condition where a “whooshing” sound is heard with each heart beat, affects over 3 million Americans, leading to anxiety, depression and even suicide1-3. While many there are many diseases associated with pulsatile tinnitus one common and serious condition is idiopathic intracranial hypertension (IIH)4. Understanding MR imaging findings in patients with pulsatile tinnitus is of the upmost interest in identifying high risk individuals for IIH. One MR finding that we hope to explore is the presence of brain herniations through arachnoid granulations into dural sinuses5 and the diagnostic utility of using these findings to understand the risk of IIH in patients with pulsatile tinnitus.Purpose
To explore if patients with pulsatile tinnitus with MR imaging findings of brain herniations through arachnoid granulations have an increased odds of having idiopathic intracranial hypertension compared to patients with pulsatile tinnitus without imaging findings of brain herniations through arachnoid granulationsMethods
Retrospective review of a cohort 262 consecutive patients who presented to our institution’s pulsatile tinnitus clinic was conducted. All patients underwent MR imaging on clinical 1.5 and 3.0T scanners including MR venogram, pre- and post-contrast T1- and T2-weighted sequences. Examinations were reviewed separately by three experienced neuroradiologists blinded to patient’s clinical data to identify the presence of brain herniations. With respect to brain herniations we documented their location, signal intensity, size, presence of arachnoid granulation, and associated dural venous sinus stenosis. All clinical records were further reviewed for documented diagnosis of idiopathic intracranial hypertension, history of prior lumbar puncture, and opening pressure. Statistical analysis was performed using a Chi Square and Odds ratio test and significance was defined as p < 0.05Results
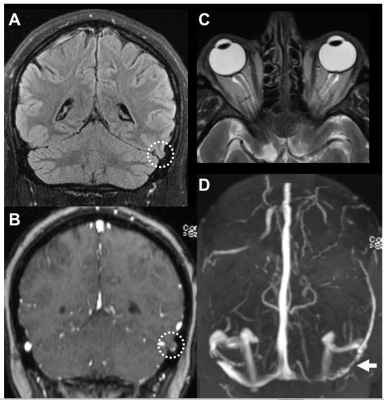
Of the entire cohort of 262 patients with pulsatile tinnitus, 16 patients (6%) were found to have at least one brain herniation through an arachnoid granulation into a dural venous sinus. 11 patients had unilateral temporal or occipital lobe herniations located in the transverse sinus or the transverse-sigmoid junction, 3 had unilateral cerebellar herniations and 2 had bilateral brain herniations with the laterality of brain herniation correlating with PT symptoms in 9 out of the 16 patients. Of the 16 patients with MRI findings of brain herniations through arachnoid granulations, 9 had a clinical diagnosis of idiopathic intracranial hypertension with 7 confirmed by LP. Of those patients without MRI findings of brain herniations through arachnoid granulations 55 patients had a clinical diagnosis of idiopathic intracranial hypertension with 39 confirmed by LP. There was a significant increased odds (OR 4.2, CI 1.5- 12) of pulsatile tinnitus patients having idiopathic intracranial hypertension with brain herniations compared to pulsatile tinnitus patients having idiopathic intracranial hypertension without brain herniations.Discussion
MR findings of brain herniations through arachnoid granulations into dural sinuses, an imaging biomarker of uncertain clinical significance, not only is higher in pulsatile tinnitus patients at 6%, compared to 1% of the general population5-6 but correlates with an increased risk for these patients of having idiopathic intracranial hypertension. Our data is the first to explore these findings in pulsatile tinnitus patients and underscores the importance of recognizing this finding on clinical brain MRI.Conclusion
Within a cohort of patients with pulsatile tinnitus, there was a significant association of brain herniations through arachnoid granulations with idiopathic intracranial hypertension. This study provides new evidence on the role of using brain herniations through arachnoid granulations as an MR imaging biomarker for diagnosis of idiopathic intracranial hypertension.Acknowledgements
No acknowledgement found.References
1. Krishnan A, Mattox DE, Fountain AJ, et al. CT arteriography and venography in pulsatile tinnitus: preliminary results. AJNR Am J Neuroradiol 2006;27:1635–38 Medline
2. Liyanage SH, Singh A, Savundra P, et al. Pulsatile tinnitus. JLaryngol Otol 2006;120:93–97 CrossRef Medline
3. Madani G, Connor SE. Imaging in pulsatile tinnitus. Clin Radiol 2009;64:319 –28 CrossRef Medline
4. Harvey RS, Hertzano R, Kelman SE, et al. Pulse-synchronous tinnitus and sigmoid sinus wall anomalies: descriptive epidemiology and the idiopathic intracranial hypertension patient population. Otol Neurotol 2014;35:7–15 CrossRef Medline
5. Liebo, G.B., et al., Brain Herniation into Arachnoid Granulations: Clinical and Neuroimaging Features. J Neuroimaging, 2016. 26(6): p. 592-598.
6. Chan, W.C., et al., Focal brain herniation into giant arachnoid granulation: A rare occurrence. European Journal of Radiology Extra, 2011. 78(2): p. e111-e113.
Figures