4925
Comprehensive MRI reveals compromised baseline cardiac function in lung cancer patients undergoing radiation therapy treatment1Medical College of Wisconsin, Milwaukee, WI, United States, 2Washington University, St Louis, MO, United States
Synopsis
Along with systemic therapies, radiation therapy (RT) plays a key role in treating lung cancer, despite high incidence of RT-induced cardiac complications. Most lung cancer patients present with cardiac risk factors that result in compromised baseline cardiac function that puts the patients at higher risk of developing cardiac complications. In this study, we investigate characteristics of baseline cardiovascular function in lung cancer patients undergoing RT. The results showed that the patients had borderline cardiac function and reduced myocardial strain measurements. Myocardial T1/T2 values in the patients were slightly high and the hemodynamic measurements showed different pattern than that in volunteers.
Introduction
Lung cancer is currently the leading cause of cancer-related death. Along with systemic therapies, radiation therapy (RT) plays a key role in treating lung cancer, although the incidence of RT-induced cardiac complications could be as high as 33%. Interestingly, many trials have not been able to correlate early deaths with clinically evident cardiotoxicity, suggesting that early non-cancer deaths may be partially due to subclinical cardiac dysfunction. Furthermore, most lung cancer patients present with cardiac risk factors that result in compromised baseline cardiac function and put the patients at higher risk of developing cardiac complications post-RT. Nevertheless, the characteristics of baseline cardiovascular function in this patient population are not well elucidated. In this study, we investigate these characteristics in lung cancer patients undergoing RT.Methods
In this IRB-approved study, six patients diagnosed with lung cancer and scheduled for RT underwent a comprehensive optimized MRI exam that included cine, tagging, T1/T2 mappings, and 4D flow sequences. Optimized parameters for cine imaging were: FIESTA acquisition, repetition time (TR) = 3.6 ms, echo time (TE) = 1.3 ms, flip angle = 55°, views per segment = 14, # averages = 1, matrix = 256×256, slice thickness = 8 mm, and readout bandwidth = 488 Hz/pixel. Optimized parameters for tagged imaging were: TR= 5.7 ms, TE = 3.1 ms, flip angle = 8°, slice thickness = 7mm, matrix = 212×192, FOV= 360×360 mm2, # averages = 1, readout bandwidth = 391 Hz/pixel, tag spacing = 7 mm. Optimized parameters for T1 mapping were: 5(3)3 MOLLI sequence, FIESTA acquisition, TR = 2:9 ms, TE = 1:3 ms, flip angle = 35°, slice thickness = 8 mm, matrix = 160×148, FOV = 360×360 mm2, # averages = 1, and readout bandwidth = 977 Hz/pixel. Optimized parameters for T2 mapping were: multi-echo spin-echo sequence, TR = 895 ms, TE = 11 − 77 ms (4 echoes with 22 ms increments), echo train length (ETL) = 16, flip angle = 90°, slice thickness = 8 mm, matrix = 180×180, FOV = 360×360 mm2, # averages = 1, readout bandwidth = 651 Hz/pixel. Optimized parameters for 4D flow were: 3D time-resolved gradient echo sequence, 3 slabs with 32 slices per slab, and 5 overlapping slices between adjacent slabs, matrix = 180×180, spatial resolution = 2 × 2 × 2:4 mm3, views per segment = 4, number of heart phases = 20, flip angle = 8°, readout bandwidth = 488 Hz/pixel, acceleration factor = 8, velocity encoding (venc) = 160 cm/s. The cine and T1/T2 images were analyzed using the cvi42 software to measure ventricular ejection fraction (EF) and T1/T2 maps, respectively. The 4D flow images were analyzed using cvi42 4D flow module to measure flow and velocity in the aorta, pulmonary artery, and mitral and tricuspid valves. The tagged images were analyzed using the SinMod-based InTag software to measure regional myocardial strain. The hemodynamic results were compared to those from two healthy volunteers. Measurements are represented as mean±SEM. Student’s t-test was used to compare measurements between patients and volunteers (P<0.05 significant).Results
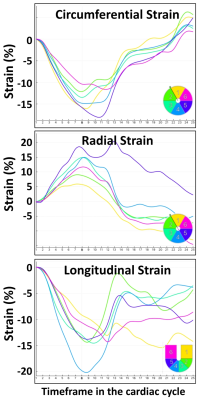
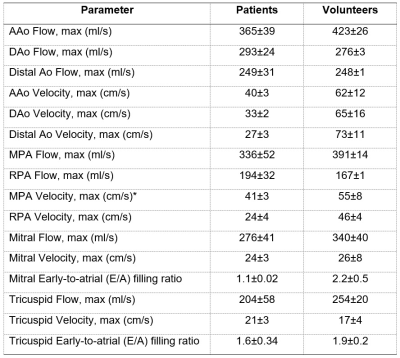
EF was normal in all patients (57±3%). All strain measurements (Figure 1) were below normal range (peak systolic strain absolute values <17%), except for the radial basal strain measurement. Basal, mid-ventricular, and apical circumferential strains were -10±0.7%, -11±1.4%, -10±1.7%, respectively. Basal, mid-ventricular, and apical longitudinal strains were -14±0.9%, -14±0.9%, -16±1.3%, respectively. Basal, mid-ventricular, and apical radial strains were 19±5.6%, 15±3.8%, 15±4.5%, respectively. Global myocardial T1 and T2 values in the patients were 1267±68 ms and 53±1.3 ms, respectively, which were slightly higher than those in the volunteers (1233±156 ms and 48±1.2 ms), but the differences were not statistically significant. Table 1 shows summary of hemodynamic measurements in both patients and volunteers. Maximum flow in the ascending aorta and main pulmonary artery in the patients were smaller than those in the volunteers, while maximum flow in the descending and distal aorta and right pulmonary artery in the patients were larger than those in the volunteers. Velocity values at all measurement sites in the patients were lower than those in the volunteers. The early-to-atrial filling ratios (E/A) measured through the mitral and tricuspid valves in the patients (1.1±0.02 and 1.6±0.34) were lower than those in the volunteers (2.2±0.51 and 1.9±0.2), although differences were not statistically significant.Discussion and Conclusions
Cardiac MRI is a valuable modality for comprehensive assessment of heart health in cancer patients. Lung cancer patients undergoing RT have borderline cardiac function and myocardial strain measurements below normal values at baseline. Myocardial T1/T2 values in the patients are slightly high and the hemodynamic measurements show different pattern than that in normal volunteers. Therefore, MRI-based baseline cardiovascular condition should be taken into consideration as a contributing factor in RT-induced cardiotoxicity and cardioprotective efforts.Acknowledgements
Study funded by Radiation Oncology Institute (ROI)References
1. D Hardy et al. Ann Oncol 2010;21:1825-33.
2. K Wang et al. J Clin Oncol 2017;35:1387-94.
3. RT Dess et al. J Clin Oncol 2017;35:1395-402.
4. EH Ibrahim. Heart Mechanics. MRI. CRC Press 2017.
Figures