4924
Motion Robust Segmented Delayed Enhancement MRI by Partially Reversed ReOrdering for GeneRal SupprESSion of Motion Induced Variable Errors1Siemens Healthineers, Durham, NC, United States, 2Duke Cardiovascular MR Center, Duke University, Durham, NC, United States
Synopsis
Standard segmented delayed enhancement (DE) is particularly motion sensitive owing to its interleaved reordering required for inversion recovery (IR). Ghosting artifacts frequently result from imperfect breath holding. The sequence cannot run free-breathing (FB). We present a novel DE technique, PROGRESSIVE, using a partially continuous reordering and dummy pulses for simultaneous motion robustness and IR-compatibility. We tested PROGRESSIVE in simulations, a motion phantom, and a cohort of patients. PROGRESSIVE images were devoid of ghosting. When acquired FB, quality was significantly better than standard DE, and equally good during perfect breath holding. PROGRESSIVE has the potential for FB self-navigated DE imaging.
INTRODUCTION
Interleaved reordering (INT) is currently the only reordering technique for segmented inversion recovery (IR) sequences[1] that, despite T1-recovery, provides excellent image quality (IQ, Fig 1a) due to a smooth k-space modulation (Fig 1b) and resulting sharp point spread function (PSF). However, INT is particularly motion-sensitive and causes ghosting artifacts during imperfect breath holding (BH) or free breathing (FB, Fig 1c). Another method, continuous reordering (CONTI) used for cine MRI is motion insensitive but causes ‘wavy’ artifacts when combined with an IR pulse (Fig 1d), due to its saw tooth modulation (Fig 1e). Interestingly, when subjected to motion, IQ of CONTI is not much worse than without motion and thus may be a useful building block for motion-robust IR imaging. To overcome its ‘waviness’ while benefiting from its motion insensitivity, we combined a partially reversed CONTI scheme with leading dummy segments (Fig 2a) to create a smooth k-space modulation (Fig 2b). This scheme, Partially Reversed ReOrdering for GeneRal SupprESSion of Motion Induced Variable Errors (PROGRESSIVE), was tested it in a simulation, a phantom, and a cohort of patients, with and without motion.METHODS
Figure 2a) shows the PROGRESSIVE scheme for N=5 shots and 25 lines per shot (LPS). Lines are acquired contiguously, in increasing phase encoding (PE) order for odd and reverse order for even numbered shots, so that the modulation discontinuities associated with CONTI are eliminated. Each data collecting segment is preceded by a dummy segment to further flatten the modulation (Fig 2b) and thus sharpen the PSF.The magnetization curves of an IR-prepared spoiled gradient echo sequence (TE 2.8ms, TR 5.0ms, effective TR 2000ms, N=5, LPS=25, matrix 256 x 125, fov 360mm x 270mm flip angle 15°, TI 430ms for INT and CONTI, TI 360ms for PROGRESSIVE) were simulated with the Bloch equations using MATLAB (MathWorks, Natick, MA). INT, CONTI, and PROGRESSIVE reordering acquired k-space data of a simulated phantom consisting of four test tubes embedded in gel with the following T1 values: fat (270ms), infarct (I, 440ms), normal myocardium (NM, 620ms), effusion (2520ms), and gel (700ms).
All schemes were implemented into a pulse sequence and tested on a 3T clinical MR scanner (MAGNETOM Vida, Siemens Healthcare, Erlangen, Germany). A motion phantom with the same T1 values as the simulation was built. In simulation and phantom, motion was simulated as a shift in PE direction (3 mm) for only one of the shots (#3). SNR was measured in I and NM. CNR between I and NM was calculated. Presence of ghosting was assessed.
In 17 cardiac patients, INT and PROGRESSIVE were run with above parameters FB to assess the effect of motion on IQ, and repeated BH for reference IQ. A blinded observer scored IQ (3 excellent, 2 good, 1 moderate, 0 nondiagnostic) and ghosting (1 present, 0 absent). IQ between INT and PROGRESSIVE was compared with a two-tailed paired t-test.
RESULTS
Figure 3 shows the phantom images for INT, CONTI and PROGRESSIVE, stationary (left column) and with motion (right column). Without motion, INT produces a sharp image but shows known discrete ghosting for effusion (long T1, arrows). CONTI shows smearing and signal ‘waviness’ in PE direction, whereas PROGRESSIVE does not. With motion, INT additionally shows the expected discrete ghosting of the test tube-to-gel interfaces, whereas CONTI and PROGRESSIVE only show signal smearing.Table 1 shows quantitative phantom and patient results. Phantom SNR and CNR for infarct and normal myocardium were similar between CONTI and PROGRESSIVE, and approximately 20% better for INT. In the patients, 11% of the BH INT and 73% of the FB INT images had ghosting. None of the PROGRESSIVE patients showed ghosting regardless of BH or FB. For BH, PROGRESSIVE and INT performed equally well. But during FB, PROGRESSIVE had significantly better IQ (1.45±0.15, p < 0.05) than INT (0.82±0.26).
Figure 4 shows images of one patient acquired with INT (top row) and PROGRESSIVE (bottom row). BH INT shows good IQ whereas FB INT exhibits strong chest wall ghosting (arrows) similar to that of an imperfect BH. The BH PROGRESSIVE image has good IQ identical to that of BH INT. During FB, PROGRESSIVE has a slightly less homogeneous blood pool than during BH but remains diagnostic, whereas INT does not.
DISCUSSION
Despite the sharp PSF and high spatial resolution of segmented INT, the frequent occurrence of motion-induced ghosting is a serious drawback and prevents segmented FB acquisitions. In patients who cannot hold their breath, currently only single shot techniques are used limiting the spatial and temporal resolution achievable. Since PROGRESSIVE is devoid of any motion-induced ghosting it may enable FB high resolution segmented IR imaging.With PROGRESSIVE we noted that, to achieve the same image contrast as for INT, shorter TI values are needed. This is likely due to the saturation by the leading dummy segments and did not limit our choice of TI.
CONCLUSION
PROGRESSIVE IQ scored significantly better than INT during FB and equally good for BH. PROGRESSIVE may allow FB navigated IR imaging with better temporal and spatial resolution than with existing FB single shot techniques with[2] or without[3] motion correction.Acknowledgements
No acknowledgement found.References
[1] Simonetti, O.P., et al., An Improved MR Imaging Technique for the Visualization of Myocardial Infarction. Radiology, 2001. 218(1): p. 215-223.
[2] Kellman, P., et al., Motion-corrected free-breathing delayed enhancement imaging of myocardial infarction. Magnetic resonance in medicine, 2005. 53(1): p. 194-200.
[3] Huber, A., et al., Single-shot inversion recovery TrueFISP for assessment of myocardial infarction. AJR Am J Roentgenol, 2006. 186(3): p. 627-33.
Figures
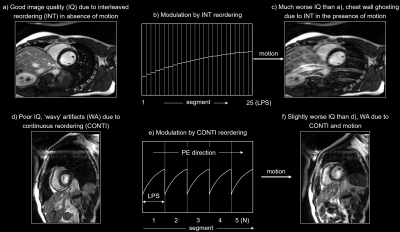
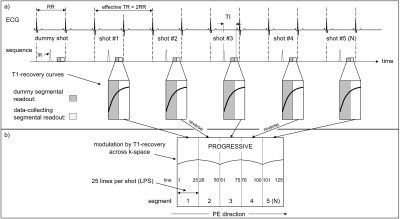
Figure 2: (a) Sequence diagram of the PROGRESSIVE technique. Each shot consists of a dummy segmental readout followed by a data-collecting readout. Both readouts consist of the same number of lines per shot. Data is read out in continuous manner to create contiguous k-space segments. The odd segments are read out with increasing phase encoding order, the others in reverse. The combination of partially reversed continuous reordering and leading dummy segments creates a smooth modulation and overcomes the ‘waviness’ of the CONTI while benefiting from its motion insensitivity.
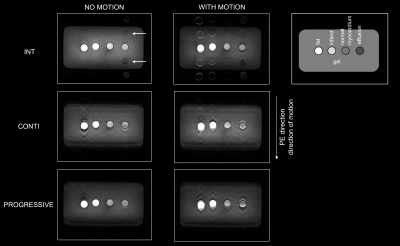
Figure 3: Phantom image results for INT, CONTI, and PROGRESSIVE reordering, in the absence (left column) and presence of motion (right column). The schematic drawing on the upper right shows the location of the test tubes relative to the gel in which they are embedded. Motion occurred in phase encoding (vertical) direction.
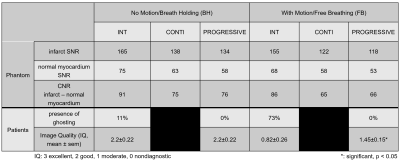
Table 1: Quantitative phantom and patient results, without motion on the left half, with motion on the right. Phantom data is shown in the top rows, patient data on the bottom. SNR in the phantom test tubes was calculated as mean of the region of interest (infarct and normal myocardium) divided by 1.5 times the standard deviation of the background noise (air).
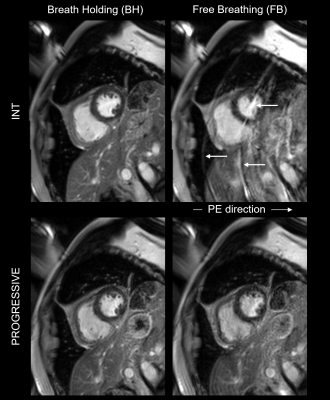
Figure 4: Images of one patient acquired with INT (top row) and PROGRESSIVE (bottom row). BH INT and PROGRESSIVE show excellent IQ. FB INT shows the known chest wall ghosting. During FB, PROGRESSIVE has a slightly less homogeneous blood pool than during BH but remains diagnostic.