4918
Heart-brain MRI evaluation in one exam: a feasibility study in healthy aging adults1Radiology, Northwestern University, Chicago, IL, United States, 2Siemens Medical Solutions Inc., Cleveland, OH, United States, 3Medical Physics, University of Greifswald, Greifswald, Germany, 4Psychiatry and Behavioral Sciences, Northwestern University, Chicago, IL, United States
Synopsis
Mechanisms underlying heart-brain hemodynamic coupling and effects on the brain remain unclear due to challenges of measuring both heart and brain in a single MRI exam. We have developed a comprehensive MRI protocol that incorporates 1) 4D flow MRI of chest, 2) 4D flow MRI of head and 3) structural neuroimaging into one MRI exam to assess cardiovascular and cerebrovascular flow as well as white matter lesions and brain atrophy. This study demonstrates the utility of heart-brain MRI as viable new tool for in vivo evaluation of hemodynamic coupling along the entire heart-brain pathway.
INTRODUCTION
Increased aortic pulse wave velocity (PWV) has been linked with white matter hyperintensities, brain atrophy and dementia risk in aging adults (1-3). However, mechanisms underlying heart-brain hemodynamic coupling and effects on the brain remain unclear due to challenges of measuring both heart and brain in a single MRI exam. 4D flow MRI is uniquely poised to systematically interrogate complex blood flow patterns along the heart-brain pathway. This technique is state-of-the-art for measuring hemodynamics in chest and head (4) and has detected increased aortic PWV with age (5-7). However, images of heart and brain are not typically acquired in the same MRI exam. Owing to advancements in imaging acceleration, 4D flow MRI can be acquired in approximately 7 minutes (heart) and 10 minutes (brain) supporting feasibility of concurrent heart-brain evaluation in a single exam. We have developed a comprehensive MRI protocol that incorporates 1) 4D flow MRI of chest, 2) 4D flow MRI of head and 3) structural neuroimaging into one MRI exam to evaluate cardiovascular and cerebrovascular flow as well as white matter lesions and brain atrophy. This study assessed the utility of this approach for evaluating age-related changes in heart-brain flow measures and relation to brain status in a small sample of healthy adults.METHODS
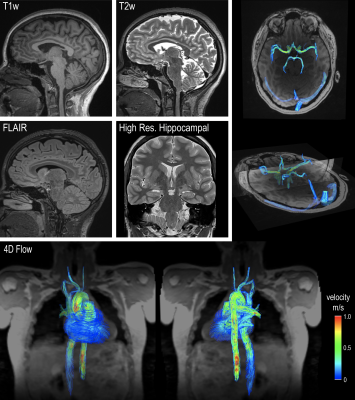
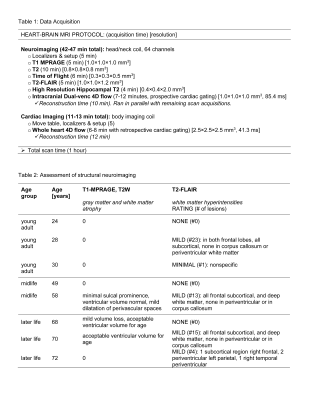
Heart-brain MRI was acquired in 8 healthy participants (5 females, age=50+/20 [24-72] years [3 young adults <45 years, 2 midlife 45-65 years, 3 later life >65 years]) at 3T (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany). Exam included the prototype free-breathing whole heart 4D flow MRI (venc=120 cm/s, compressed sensing R=10.2), intracranial dual-venc 4D flow MRI (venc=50 cm/s and 100 cm/s, k-t GRAPPA R=5) and structural neuroimaging (T1-MPRAGE, T2W, high resolution hippocampal T2W, T2-FLAIR, TOF MRA) (Figure 1, Table 1). Participants were screened for history of cardio- and cerebrovascular problems that may influence blood flow. Exclusion criteria: BMI>40, blood pressure>160/90 mmHg, heart or brain surgery, stroke, brain injury, seizures, coma, diabetes, cancer, liver or kidney disease, arrhythmia, regular smoking, or drug abuse. Blood pressure was recorded 3 times before and 3 times after scan and averaged. Imaging workflow is shown in Figure 2. Whole heart 4D flow MRI was analyzed using a previously established workflow (5). Briefly, 4D flow MRI data was preprocessed including calculation of time-averaged 3D phase contrast angiogram (PC-MRA). Aorta was segmented from PC-MRA and PWV was evaluated using cross-correlation algorithm with repeated approach. Intracranial 4D flow MRI was analyzed using a previously established workflow (8,9). Briefly, PC-MRA was used to segment vessels of interest including the basilar artery (BA), left and right intracranial arteries (LICA, RICA) and left and right middle cerebral arteries (LMCA, RMCA). Analysis planes were automatically placed every 1 mm. For each vessel, pulsatility index (PI) and resistive index (RI) were determined for each analysis plane and median gave final value. Results for bilateral vessels were averaged. Structural neuroimaging data was reviewed by an expert neuroradiologist (ER) for brain atrophy (T1-MPRAGE, T2W), hippocampal atrophy (high resolution hippocampal T2W), white matter lesions (T2-FLAIR) and narrowed arteries (TOF).RESULTS
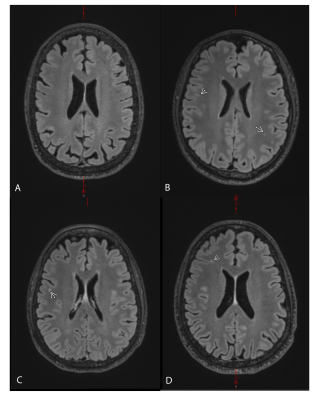
Increasing aortic PWV was significantly correlated with age (r=0.71, p=0.048) (n=8) (Figure 3). Increasing ICA PI (r=0.91, p=0.032) and ICA RI (r=0.91, p= 0.034) were highly correlated with age in midlife and later life participants (n=5). White matter hyperintensities were rated clinically mild in 4 of the 8 participants (1 young, 1 midlife and 2 later life participants) (Figure 4, Table 2); all were subclinical mild punctate foci (<2 mm diameter) with no confluence. There were no neuroradiological findings of brain atrophy in gray matter or white matter overall or in hippocampus; ventricular dilation, where present, was considered acceptable for participant age. There were no neuroradiological findings for narrowed arteries. Increased systolic blood pressure (SBP) and pulse pressure (PP) correlated with higher number of white matter lesions (SBP: r=0.75, p=0.034, PP: r=0.80, p=0.018).DISCUSSION
This study supports the feasibility of acquiring heart-brain MRI data in a single exam for the comprehensive analysis of heart-brain coupling. This approach enabled systematic evaluation of aging along the heart-brain pathway. Aortic PWV increased across the adult lifespan confirming previous results (5-7). Cerebrovascular pulsatility in internal carotids was highly correlated with aging in midlife to later life adults. Also, increased blood pressure was related to number of white matter hyperintenstities as shown in other studies, e.g. (10). White matter lesions, considered a marker of small vessel disease, are common findings on T2-FLAIR and often found in healthy individuals. Taken together, this supports the utility of this approach for investigating heart-brain hemodynamic coupling in clinically silent periods of the adult lifespan to inform an understanding of factors influencing neurological outcome in older age.CONCLUSION
This study demonstrates heart-brain MRI as a promising new tool for evaluation of hemodynamic coupling along the entire heart-brain pathway. This approach provides new capabilities for studying age-related changes by capturing in vivo measures of 4D flow MRI-derived aortic PWV, 4D-flow MRI-derived cerebrovascular pulsatility and T2-FLAIR assessment of white matter lesions in one MRI exam. Future study in larger cohorts, including individuals with cardiovascular risk factors is warranted.Acknowledgements
Grant support by Funding Sources: NIH NIA T32AG020506, P30AG072977; NINDS R21NS122511References
1. Pase MP, Beiser A, Himali JJ, Tsao C, Satizabal CL, Vasan RS, Seshadri S, Mitchell GF. Aortic Stiffness and the Risk of Incident Mild Cognitive Impairment and Dementia. Stroke; a journal of cerebral circulation 2016;47(9):2256-2261.
2. Rosano C, Watson N, Chang Y, Newman AB, Aizenstein HJ, Du Y, Venkatraman V, Harris TB, Barinas-Mitchell E, Sutton-Tyrrell K. Aortic pulse wave velocity predicts focal white matter hyperintensities in a biracial cohort of older adults. Hypertension (Dallas, Tex : 1979) 2013;61(1):160-165.
3. Sala M, van den Berg-Huysmans A, van der Grond J, Huisman M, Brandts A, Westenberg JJ, de Roos A. Aortic Arch Stiffness Is Associated With Incipient Brain Injury in Patients With Hypertension. Am J Hypertens 2016;29(6):705-712.
4. Dyverfeldt P, Bissell M, Barker AJ, Bolger AF, Carlhall CJ, Ebbers T, Francios CJ, Frydrychowicz A, Geiger J, Giese D, Hope MD, Kilner PJ, Kozerke S, Myerson S, Neubauer S, Wieben O, Markl M. 4D flow cardiovascular magnetic resonance consensus statement. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance 2015;17(1):72.
5. Jarvis K, Soulat G, Scott M, Vali A, Pathrose A, Syed AA, Kinno M, Prabhakaran S, Collins JD, Markl M. Investigation of Aortic Wall Thickness, Stiffness and Flow Reversal in Patients With Cryptogenic Stroke: A 4D Flow MRI Study. J Magn Reson Imaging 2021;53(3):942-952.
6. Harloff A, Mirzaee H, Lodemann T, Hagenlocher P, Wehrum T, Stuplich J, Hennemuth A, Hennig J, Grundmann S, Vach W. Determination of aortic stiffness using 4D flow cardiovascular magnetic resonance - a population-based study. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance 2018;20(1):43.
7. Soulat G, Gencer U, Kachenoura N, Villemain O, Messas E, Boutouyrie P, Laurent S, Mousseaux E. Changes in segmental pulse wave velocity of the thoracic aorta with age and left ventricular remodelling. An MRI 4D flow study. Journal of hypertension 2020;38(1):118-126.
8. Aristova M, Vali A, Ansari SA, Shaibani A, Alden TD, Hurley MC, Jahromi BS, Potts MB, Markl M, Schnell S. Standardized Evaluation of Cerebral Arteriovenous Malformations Using Flow Distribution Network Graphs and Dual-venc 4D Flow MRI. J Magn Reson Imaging 2019;50(6):1718-1730.
9. Vali A, Aristova M, Vakil P, Abdalla R, Prabhakaran S, Markl M, Ansari SA, Schnell S. Semi-automated analysis of 4D flow MRI to assess the hemodynamic impact of intracranial atherosclerotic disease. Magn Reson Med 2019;28(10):27747.
10. Verhaaren BF, Vernooij MW, de Boer R, Hofman A, Niessen WJ, van der Lugt A, Ikram MA. High blood pressure and cerebral white matter lesion progression in the general population. Hypertension (Dallas, Tex : 1979) 2013;61(6):1354-1359.
Figures