4915
Cine MRI detects shorter cardiac rest periods in pulmonary hypertension1Radiology, Northwestern University, Chicago, IL, United States
Synopsis
The existence of pulmonary hypertension (PH) can independently shorten the length of cardiac rest periods. The length of cardiac rest periods can be used to discriminate PH patients from healthy controls.
Background
Cardiac rest periods refer to time intervals in a cardiac cycle when the cardiac motion is minimal, and the ventricles are nearly “frozen”. Cardiac rest periods serve as optimal acquisition windows for magnetic resonance imaging (MRI) examinations that are sensitive to cardiac motion. Typically located in the end-systole and the middle to late-diastole, cardiac rest periods are formed during transition courses between adjacent contraction and dilation modes of the ventricles. Therefore, changes of systolic and diastolic properties are expected to disturb the temporary myocardial “quiescence” and reshape the rest periods. Unfortunately, the length of cardiac rest periods was traditionally used as a technical factor for adjusting imaging parameters. Its clinical relevance has not been reported.Purpose
To test the hypothesis that the existence of pulmonary hypertension (PH) alters the length of cardiac rest periods.Materials and methods
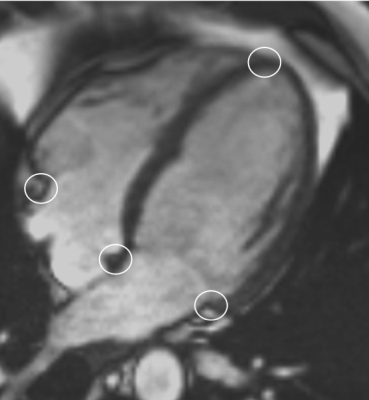
With the approval of institution review board (IRB), 51 consecutive PH patients (21 males, 33 – 83 years old, diagnosed with right heart catheterization [RHC]) and 24 healthy volunteers (15 males, 26 – 80 years old) were recruited to undergo MRI scans. The length of cardiac rest fields was measured on cine MRI (at four-chamber view) and expressed as relative/absolute lengths and rest ratios. Figure 1. The lengths of rest periods were compared between participant groups. Multiple linear models (MLR) were used to find Influences of the length of cardiac rest periods. Receiver operation curve (ROC) was used to estimate the capability of the length of cardiac rest periods in predicting PH.Results
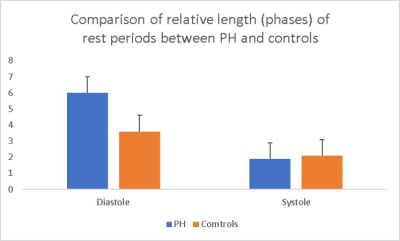
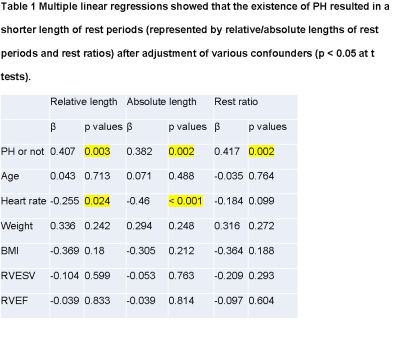
Compared to health controls, PH patients were older (59.1 ± 13.6 years vs. 51.8 ± 13.8 years, p = 0.032) and they had higher bodyweight (92.1 ± 23.2 Kg vs. 76.8 ± 17.3 Kg, p = 0.006), BMI (32.2 ± 6.9 vs. 26 ± 4.9, p < 0.001), heart rates (76.5 ± 9.1 vs. 69.5 ± 9.3, p = 0.021), RVESV (89.2 ± 41 vs. 67.6 ± 20.7, p = 0018), lower RVEF (47.1 ± 12.1 % vs. 56 ± 5.6 %, p = 0.001), shorter relative (3.6 ± 2.1 phases vs. 6 ± 1.3 phases, p < 0.001) and absolute (120.6 ± 77.2 ms vs. 212.5 ± 60.2 ms, p < 0.001) lengths of cardiac rest periods and lower rest ratios (0.21 ± 0.1 vs. 0.44 ± 0.1, p < 0.001 ) in diastole. While there was no difference on other indices, including the length of rest periods in end-systole. Figure 2.There were strong correlations among relative and absolute lengths and rest ratios at diastole (r > 0.9, p < 0.05). However, only absolute length of rest periods at diastole had a moderate correlation with heart rates (r = -0.571, p < 0.001). Using multi-variate linear models, we found that the status of PH independently contributed to a shorter cardiac rest period (relative and absolute) and rest ratio at diastole after the adjustment of age, heart rate, body weight, BMI, RVESF and RVEF. Table 1.
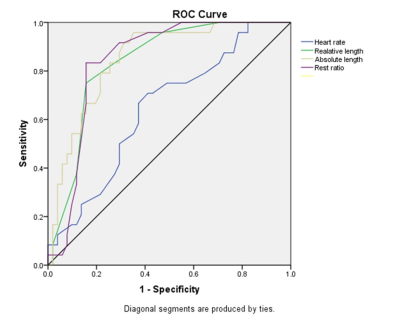
ROC curves showed that relative (AUC = 0.838, 95% CI = 0.747 – 0.929) and absolute (AUC = 0.851, 95% CI = 0.764 – 0.939) lengths of rest periods and rest ratios (AUC = 0.845, 95% CI = 0.755 – 0.939) at diastole had better performance (Z tests, p < 0.05) than the heart rate (AUC = 0.643, 95%CI = 0.513 – 0.773) in discriminating PH patients from controls. Figure 3.
Discussion
In the present study, we demonstrated that the existence of PH independently resulted in a significant reduction of cine MRI-derived cardiac rest periods in diastole after the adjustment of prominent covariates, including age and heart rates. The length of cardiac rest periods could effectively discriminate PH patients from controls. As such, a shorter cardiac rest period was found no longer just an adverse physical condition for cardiac imaging. It has the potential to become a novel imaging biomarker of CVDs.In addition to establishing the role of the length of cardiac rest periods in the assessment of CVDs, our results might also draw attentions from developers of cardiac imaging techniques. Since CVDs could be another prominent source of a short rest period, it should be caution that some imaging techniques which are originally developed on healthy volunteers may encounter extra difficulties in CVDs patients with shorter rest periods.
Our study has limitations. First, we only measured cardiac rest periods on 4-chamber view cine MRI because both LV and RV were fully visible on this standard view. Therefore, the motion perpendicular to the imaging plane could be missed. Second, compared to clinical echocardiography, the temporal resolution of cine MRI protocol in the present study was low. With 25 phases per cardiac cycle, we were unable to detect possible subtle differences of rest periods, especially at the end-systole.
Conclusion
PH is independently associated with shorter cardiac rest periods in diastole. The length of cardiac rest periods has the potential to become a novel quantitative imaging biomarker for presenting cardiovascular health.Acknowledgements
No acknowledgement found.References
1. Lin K, Lloyd-Jones DM, Liu Y, Bi X, Li D, Carr JC. Noninvasive evaluation of coronary distensibility in older adults: a feasibility study with MR angiography. Radiology. 2011;261(3):771-8.
2. Lin K, Lloyd-Jones DM, Liu Y, et al. The role of latency period in quality management for free-breathing coronary wall MRI. Int J Cardiovasc Imaging. 2015;31(3):621-7.
3. Shechter G, Resar JR, McVeigh ER. Rest period duration of the coronary arteries: implications for magnetic resonance coronary angiography. Med Phys. 2005;32(1):255-62.
4. Wang Y, Vidan E, Bergman GW. Cardiac motion of coronary arteries: variability in the rest period and implications for coronary MR angiography. Radiology. 1999;213(3):751-8.
5. Lu B, Mao SS, Zhuang N, et al. Coronary artery motion during the cardiac cycle and optimal ECG triggering for coronary artery imaging. Investigative radiology. 2001;36(5):250-6.
6. Rose-Jones LJ, McLaughlin VV. Pulmonary hypertension: types and treatments. Current cardiology reviews. 2015;11(1):73-9.
7. Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. The European respiratory journal. 2019;53(1).
8. Vinnakota KC, Bassingthwaighte JB. Myocardial density and composition: a basis for calculating intracellular metabolite concentrations. American journal of physiology Heart and circulatory physiology. 2004;286(5):H1742-9.
9. Aronson D, Eitan A, Dragu R, Burger AJ. Relationship between reactive pulmonary hypertension and mortality in patients with acute decompensated heart failure. Circulation Heart failure. 2011;4(5):644-50. 10. Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function--a study in normals and dilated cardiomyopathy. Journal of cardiology. 1995;26(6):357-66.
11. Harjai KJ, Scott L, Vivekananthan K, Nunez E, Edupuganti R. The Tei index: a new prognostic index for patients with symptomatic heart failure. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2002;15(9):864-8.
12. Shingu Y, Amorim P, Nguyen TD, Mohr FW, Schwarzer M, Doenst T. Myocardial performance (Tei) index is normal in diastolic and systolic heart failure induced by pressure overload in rats. European journal of echocardiography : the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2010;11(10):829-33.
13. Rovno HD, Litt H, Ferrari VA. MRI assessment of myocardial global function by tei index - a comparison to echocardiographic tei index. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2011;13.
14. Lin K, Sarnari R, Pathrose A, et al. Cine MRI detects elevated left heart pressure in pulmonary hypertension. Journal of magnetic resonance imaging : JMRI. 2021.
Figures