4884
Myocardial first-pass perfusion assessed by cardiac magnetic resonance and neutrophil to lymphocyte ratio in patients with cardiac syndrome X
Gang zhang1, Wei Xing1, Tingting Li2, Yan Zheng1, Ying Huang3, Junjing He1, and Xiuzheng Yue4
1Department of Magnetic Resonance, The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 2Department of Magnetic Resonance, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou, China, 3The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 4Philips Healthcare, Zhengzhou, China
1Department of Magnetic Resonance, The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 2Department of Magnetic Resonance, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou, China, 3The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 4Philips Healthcare, Zhengzhou, China
Synopsis
Cardiac syndrome X (CSX) is also known as microvascular angina pectoral, the pathogenesis of which has not been clearly determined [1]. A coronary angiography study [2] showed that neutrophil to lymphocyte ratio (NLR), as a marker of inflammatory response in a variety of cardiovascular diseases, was elevated in CSX patients. The NLR of CSX patients with impaired myocardial perfusion was higher than that of patients without it, such as unstable angina pectoris (UAP) patients. In this study, we found that the distribution of myocardial first-pass perfusion was heterogeneous in each segment of CSX patients in the resting stage, better than that of UAP patients. The correlation between perfusion parameters and NLR was high and significant.
Introduction
Cardiac syndrome X is a common clinical disease, and its possible pathogenesis includes: impaired endothelial function of coronary artery, inflammatory response, estrogen deficiency, etc. The neutrophil to lymphocyte ratio is a common inflammatory marker of cardiovascular disease, which can be extracted simply from the whole blood cell count. Moreover, NLR is better than other white blood cell subsets in predicting the severity of cardiovascular disease [3,4]. There are a few studies on the correlation between NLR and myocardial perfusion in CSX patients. Okyay K[2] investigated CSX patients with coronary angiography, and the results showed that NLR of CSX patients with impaired myocardial perfusion was higher, suggesting that inflammation may be involved in myocardial ischemia of CSX patients. MR myocardial perfusion imaging has been proved it can accurately detect the location and range of myocardial ischemia [5]UAP patients had coronary artery stenosis > 40%, and the vascular stenosis was the main factor causing poor myocardial perfusion. CSX patients had no severe coronary artery stenosis or occlusion, and microvascular dysfunction was the main factor causing poor myocardial perfusion. To investigate the relationship between inflammatory response and myocardial perfusion in CSX patients, we assess the cardiac perfusion parameters of patients with CSX and UAP in resting state, and further evaluated its correlation with NLR.Methods
Twenty-five patients (12 CSX patients including 3 males and 9 females, mean age: 47.6 ± 10.9; 13 AUP patients including 8 males and 5 females, mean age: 61.6 ± 7.6) were prospectively enrolled into this study from January 2017 to October 2021. All patients underwent exercise treadmill test and coronary angiography within one week.CMR examinationCMR: imaging was performed on a Ingenia 3.0T scanner (philips, Netherlands) in a head-first supine position with a 32-channel coil. Myocardial first pass perfusion imaging: GD-DTPA (0.1 mmol/kg) was injected into the venous channel as a bolus (rate of 4 ml/s) . After injection, three short-axis slices (apical, mid-ventricular and basal) were obtained with dynamic multi-cycle scan. The settings for scanning sequence FFE were as follows: FOV 300×300mm, reconstruction matrix 224×224, slice thickness 10mm. TE shortest value, TR shortest value, flip angle 15°, sense factor 2.3.CMR Analysis: All CMR analysis was performed by using commercial software CVI42 version 5.2 (Circle Cardiovascular Imaging Inc., Calgary, Canada). The left ventricular apex, middle, and base, the boundaries of the myocardium, and the epicardium were manually traced, and the blood pool and papillary muscle were excluded. The software automatically calculates perfusion index.Statistical analysis: Measurement data were expressed as mean ± standard deviation, and differences in variables between CSX and UAP were examined with t test. Counting data were expressed as ratio, difference was tested with χ2 test. The relationship between NLR and perfusion parameters was evaluated by Person correlation coefficient. P<0.05 was considered statistically significant.Results
12 CSX (3M,9F) patients and 13 UAP (8M,5F) patients were screened with complete data. Detailed information of patients is shown in Table 1. There were significant differences only in age between each two groups.Distribution of perfusion parameters in CSX patientsThe perfusion parameters of each segment are distributed heterogeneously in CSX patients. As shown in Table 2.There were differences in perfusion parameters and NLR between CSX patients and UAP patients, as shown in Table 3.As shown in Table 4, slope/baseline signal intensity, peak time, 20%-80% peak time, or maximum signal intensity/baseline signal intensity of CSX patients were highly correlated with NLR, with p value<0.05.UAP patients were not associated with NLR.Discussion
Retrospective analysis of 12 CSX patients with myocardial first pass perfusion shows that the distribution of cardiac perfusion parameters is heterogeneous in 16 segments in the resting stage. This result indicates that although myocardial ischemia is relatively mild in CSX patients, the perfusion insufficient of the myocardium in resting stage can still be displayed in the first pass perfusion of cardiac MRI, while the perfusion distribution of the myocardium in CSX patients is heterogeneous. The data in this study showed that the NLR of CSX patients was larger than that of UAP patients, which represented a more severe inflammatory response, consistent with previous researchers, indicating that inflammatory response may be involved in the occurrence and development of CSX. However, CSX patients had better myocardial perfusion status than UAP patients. The possible reason is the deterioration of myocardial perfusion caused by coronary artery stenosis in UAP patients. The results showed that myocardial perfusion parameters were highly correlated with NLR (P < 0.05), indicating that inflammatory response of CSX patients was aggravated, and myocardial perfusion decreased. We demonstrated the close negative correlation between NLR and myocardial perfusion in CSX patients, thus suggesting that inflammatory response causes myocardial ischemia and participates in the occurrence and development of CSX course.Conclusion
CMR first-pass perfusion can reveal myocardial ischemia in patients with CSX in the resting stage. In CSX patients, there was a negative correlation between myocardial perfusion and NLR, which suggested that inflammatory response caused myocardial ischemia, further indicating that inflammatory response plays an important role in the occurrence and development of CSX.Acknowledgements
No acknowledgement found.References
1. Ibrahim H Altiparmak,Muslihittin E Erkus,Hatice Sezen,et al. Evaluation of thiol levels, thiol/disulfide homeostasis and their relation with inflammation in cardiac syndrome X. Coron Artery Dis.2016;27:295-301.2. Okyay K, Yilmaz M, Yildirir A,et al.Relationship between neutrophil to lymphocyte ratio and impaired myocardial perfusion in cardiac syndrome X.Eur Rev Med Pharmacol Sci.2015;19:1881-1887.3. Xavier N D D, Nandan S B, Jayachandran P R, et al.Chronic effects of copper and zinc on the fish,Etroplus swatensis ( Bloch, 1790 ) by continuous flow through (CFT) bioassay.Mar Environ Res.2019;143:141-157.4. Charnese B, Michael R, Malyka Y, et al.Coronin 1A depletion restores the nuclear stability and viability of Aip1 / Wdr1-deficient neutrophils.J of Cell Biol.2019;218: 3258-3271.5. Liu A, Wijesurendra RS, Liu JM,et al.Diagnosis of Microvascular Angina Using Cardiac Magnetic Resonance. J Am Coll Cardiol.2018;71:969–979.Figures
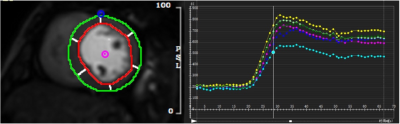
Figure 1. Semi-quantitative analysis of CMR perfusion. Contours are drawn reflecting the epicardium and endocardium dividing the myocardium in six segments per slice. Below are signal intensities given in relation to time for the six segments (dark green, light green, pink, yellow, dark blue, light blue) and the blood pool (orange) illustrating the appearance and uptake of gadolinium
Table 1. A summary for the clinical data of patients
Table 2. Perfusion parameters of 16 segments in CSX patients
Table 3. Perfusion parameters and NLR between CSX and UAP patients
Table 4. Correlation analysis of perfusion parameters and NLR
DOI: https://doi.org/10.58530/2022/4884