4851
Bariatric Surgery increases Cerebral Blood Flow in Women with Obesity1Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Obesity is a significant risk factor for cerebrovascular disease including dementia. Cerebral blood flow (CBF) provides a biomarker of cerebrovascular health and can be measured non-invasively using arterial spin labeled (ASL) perfusion MRI. Here we examined longitudinal ASL data from adult women with obesity who underwent bariatric surgery. We demonstrated that weight loss was associated with significant increases in CBF from baseline to 6 and 18 months after surgery. Change in glucose and insulin level did not mediate the relationship, suggesting a more direct association between obesity and CBF.
Introduction
Obesity is a significant risk factor for cerebrovascular disease including dementia.1 A number of mechanisms linking adiposity to dementia have been proposed such as vascular insufficiency, inflammation, type 2 diabetes and hyperinsulinemia that may collectively contribute to the overall dementia risk.2–4 Obesity is also associated with reduced cerebral blood flow,5 which can contribute to the occurrence of future dementia due to suboptimal maintenance of basal function and impaired cerebrovascular health. Here, we examined longitudinal magnetic resonance brain imaging data from women undergoing bariatric surgery and assessed if their weight loss would increase CBF post-surgery.Method
Surgery participants for this study (Clinical Trials registration number NCT01228097) were recruited from the Penn Metabolic and Bariatric Surgery Program and the Center for Weight and Eating Disorders at the University of Pennsylvania. Inclusion criteria included female gender, age≥18 years, and a body mass index (BMI)≥40 kg/m2 (or BMI≥35 kg/m2 with significant weight related comorbidities). Participants, in consultation with their surgeon, elected to undergo either vertical sleeve gastrectomy (VSG, N=19) or Roux-en-Y gastric bypass (RYGB, N=25), the two commonly used surgical procedures for weight loss, and were referred to the study in consecutive order.6 25 women with similar characteristics as surgery candidates who were willing to remain weight stable (within 5% baseline weight) for the next 18 months were recruited as the non-surgical control group.The MRI data were acquired on a Siemens 3T scanner pre-surgery (baseline) and at 6 and 18 months post-surgery. The protocol included 2D pseudo continuous ASL using a labeling time/post labeling delay of 1.5s/1.2s, and voxel size= 2.3x2.3x6mm3. ASL derived mean CBF7,8 in the whole brain was used for further analysis. Changes in CBF from baseline to 6 and 18 months were compared between the surgical groups and controls and were also correlated with change in BMI, fasting glucose and insulin level (available in N=64, 61 and 59 participants respectively). Finally, we used a mediation analysis to assess if change in glucose or insulin level explained the relationship between BMI and CBF changes.
Results
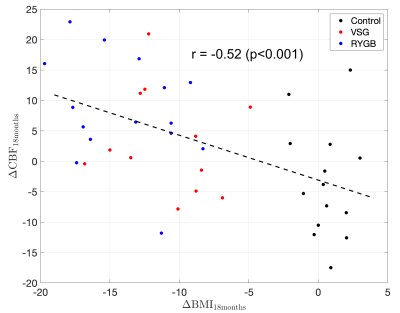
The demographic characteristics of the three groups at baseline, 6 months and 18 months follow-up are shown in Table 1. There were no differences in age and BMI between the three groups at baseline. Participants undergoing surgery had a significant decrease (p<0.0001) in BMI at both 6 and 18 months compared to the controls. There was no significant difference in reduction in BMI in the two surgical groups, though there was a trend (p=0.08) of greater reduction in BMI in RYGB than VSG at 18 months follow-up.Mean whole brain CBF at the three time points is shown in Table 1. The participants undergoing surgery showed significantly increased CBF compared to the controls after 6 and 18 months (p<0.0001 and p=0.01 respectively). When considered separately, both the surgical groups showed significantly increased CBF compared to the controls (p=0.002 in VSG, p<0.0001 in RYGB) after 6 months. However, at 18 months, only the RYGB group showed increased CBF compared to the controls (p=0.005). The groups did not differ in CBF changes from 6 to 18 months, similar to the trend of BMI reduction which also occurred mostly in the first 6 months. Pooling all participants, the changes in CBF from baseline to 6 or 18 months were negatively associated with the changes in BMI (r = -0.58 and -0.52 respectively, p<0.001, scatter plot for change in 18 months is shown in Figure 1).
Table 1 also lists the fasting glucose and insulin levels in all the participants. Compared to the controls, both the surgery groups showed significant reduction in glucose level at 6 and 18 months and also in insulin level (except RYGB at 18 months follow-up). The changes in glucose correlated with the corresponding CBF changes from baseline to 6 months (r=-0.29, p=0.04) and 18 months (r=-0.49, p=0.003). The correlation between changes in insulin level and CBF showed trends for both the time points (p<0.07). None of these changes mediated the relationship between the BMI and CBF changes.
Discussion
Weight loss with bariatric surgery increased CBF, resulting in potentially improved cerebrovascular health. Fasting glucose or insulin levels did not mediate the relationship suggesting a more direct relationship between obesity and CBF. In human childhood and adolescence, the ratio of brain and body metabolism varies across different phases of brain and body development, suggesting a brain-body competition for metabolic substrate.9,10 Competition for metabolic substrate between brain and body might also exist in adulthood, and redistribution of substrate with weight loss after bariatric surgery could explain observed increases in CBF. The CBF changes were different in the two surgical groups and could be due to the differences in the achieved BMI. CBF in the control group unexpectedly decreased at 6 months and then remained stable, which also contributed to the observed CBF differences between surgery and controls. Interestingly, fasting glucose in controls also showed an unexpected increase between baseline and 6 months, suggesting the possibility that fasting glucose may be a determinant of CBF when BMI remains stable.Conclusion
Increased CBF was observed in women with obesity after bariatric surgery and may represent a benefit of bariatric surgery for cerebrovascular health.Acknowledgements
NIH grants R01 DK085615, R01 NS111115, and R03 AG063213 and K23 NR017209.References
1. Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: A meta-analysis of prospective studies. Obes Rev. 2011;12(5):426-437. doi:10.1111/j.1467-789X.2010.00825.x
2. Kivipelto M, Ngandu T, Fratiglioni L, et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol. 2005;62(10):1556-1560. doi:10.1001/archneur.62.10.1556
3. Luchsinger JA, Gustafson DR. Adiposity, type 2 diabetes, and Alzheimer’s disease. J Alzheimer’s Dis. 2009;16(4):693-704. doi:10.3233/JAD-2009-1022
4. Kiliaan AJ, Arnoldussen IAC, Gustafson DR. Adipokines: A link between obesity and dementia? Lancet Neurol. 2014;13(9):913-923. doi:10.1016/S1474-4422(14)70085-7
5. MacIntosh BJ, Shirzadi Z, Atwi S, et al. Metabolic and vascular risk factors are associated with reduced cerebral blood flow and poorer midlife memory performance. Hum Brain Mapp. 2020;41(4):855-864. doi:10.1002/hbm.24844
6. Alamuddin N, Vetter ML, Ahima RS, et al. Changes in Fasting and Prandial Gut and Adiposity Hormones Following Vertical Sleeve Gastrectomy or Roux-en-Y-Gastric Bypass: an 18-Month Prospective Study. Obes Surg. 2017;27(6):1563-1572. doi:10.1007/s11695-016-2505-5
7. Dolui S, Wang Z, Shinohara RT, Wolk DA, Detre JA. Structural Correlation-based Outlier Rejection (SCORE) algorithm for arterial spin labeling time series. J Magn Reson Imaging. 2017;45(6):1786-1797. doi:10.1002/jmri.25436
8. Alsop DC, Detre JA, Golay X, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2015;73(1):102-116. doi:10.1002/mrm.25197
9. Kuzawa CW, Chugani HT, Grossman LI, et al. Metabolic costs and evolutionary implications of human brain development. Proc Natl Acad Sci U S A. 2014;111(36):13010-13015. doi:10.1073/pnas.1323099111
10. Vandekar SN, Shou H, Satterthwaite TD, et al. Sex differences in estimated brain metabolism in relation to body growth through adolescence. J Cereb Blood Flow Metab. 2019;39(3):524-535. doi:10.1177/0271678X17737692