4830
Comparison of RF-Induced Heating of a Vascular Stent in an ASTM Phantom and Two Virtual Human Anatomies in Open and Closed Bore MRI Systems1MED Institute Inc., West Lafayette, IN, United States
Synopsis
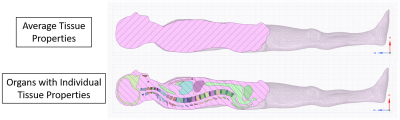
The primary goal of this study was to compare radiofrequency (RF) induced temperature rises of a stent within the ASTM phantom and two virtual human anatomies in a 1.2 T Hitachi Oasis open bore, 1.5 T Siemens Altea closed bore, and 3.0 T Siemens Prisma closed bore MRI systems for the purpose of MRI labeling according to ASTM F25031. The secondary goal was to simulate RF-induced heating of the same stent within the Duke virtual human model containing 1) internal organs with individual material properties and 2) no internal organs and average tissue properties throughout and compare predicted temperature rises.
Purpose
Open bore MRI systems have several advantages over closed bore MRI systems including the wide patient table, the ability to scan larger patients, and open field of view2. These benefits allow for the imaging of pediatric, bariatric, geriatric, and claustrophobic patients. With the growing number of open bore MRI systems, it is of paramount importance to understand the effects of RF-induced heating on metallic medical devices. The purpose of this abstract is to demonstrate how a device (e.g. vascular stent) that has a relatively high temperature rise in closed bore systems can have a potential safety advantage (i.e., lower temperature rise) in an open bore system. RF-heating results in two virtual human anatomies were compared, one with internal organs with individual material properties, and the other without internal organs and with average tissue properties throughout.Methods
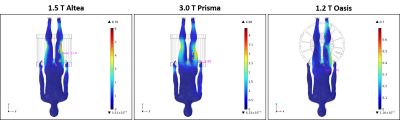
COMSOL Multiphysics® was used to build computational models for the 1.2 T Hitachi Oasis open bore MRI system, 1.5 T Siemens Altea closed bore MRI system, and the 3.0 T Siemens Prisma closed bore MRI system. All three models were built using geometric details provided by Hitachi (Fujifilm) and Siemens. Figure 1 shows each MRI system and the RF body coils with the Duke human anatomy model. Validation of each computational model included RF-induced heating measurements of titanium calibration rods in the ASTM F2182 phantom. Input voltages for simulations were tuned to generate a whole phantom SAR of 2 W/kg in each MRI system. RF-induced heating simulating a 15-minute scan of a Nitinol superficial femoral artery (SFA) stent in an ASTM phantom, as well as two Duke human virtual anatomies was conducted. The gel phantom was assumed to be a solid, therefore convective heat transfer in the gel was not considered since the viscosity of the gel prevents bulk fluid motion. Stents were positioned 2 cm from the bottom of each ASTM phantom, as higher heating is associated with this location in the open bore MRI system. The stent in the open bore MRI system was positioned in the center of the phantom, as this location was associated with a region of known electric field, in accordance with ASTM F21823. Material properties pertaining to heat transfer for individual internal organs were taken from the IT’IS database4 and assigned to each organ as shown in Figure 4. Average tissue properties were assumed to be the same as the gelled saline, according to ASTM F21823.Results and Discussion
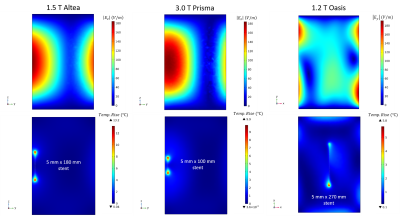
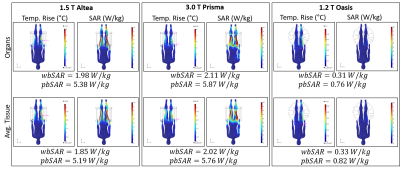
The electric field associated with the closed bore scanners with no device appear similar in terms of both tangential (z-direction) electric field component magnitude as well as overall contour (Figure 2). However, the tangential (y-direction) component magnitude is lower in the open bore system. Different length stents were tested in each scanner within the ASTM phantom, with the length corresponding to the resonant wavelength of each individual scanner (i.e., frequency), thus providing the maximum expected temperature rise. The 1.5 T Siemens Altea demonstrated the highest heating in the ASTM phantom at 13.2°C, followed by the 3.0 T Siemens Prisma (9.9°C), and the 1.2 T Hitachi Oasis (5.8°C). Figure 3 shows trends for RF-induced heating in the virtual human anatomy containing internal organs with individual material properties with a stent, which followed a similar trend (11.0°C, 7.0°C, 1.5°C). Simulated temperature rises and overall contours were comparable between the two virtual human anatomies, with similar predicted whole-body and partial-body SAR values. This indicates the human anatomy with average tissue properties throughout the anatomy without internal organs is able to predict accurate temperature rises while significantly lowering computational cost.Conclusions
A Nitinol SFA stent was compared in terms of RF-induced heating in the ASTM phantom, as well as two virtual human anatomies in the 1.2 T (49 MHz) Hitachi Oasis open bore system, the 1.5 T (64 MHz) Siemens Altea closed bore system, and the 3.0 T (128 MHz) Siemens Prisma closed bore system. Results demonstrated a device with a relatively high temperature rise in closed bore MRI systems could have a potential safety advantage (i.e., lower temperature rise) in an open bore MRI system. In terms of the comparison of the two virtual human anatomies, simulated temperature rises and SAR values were similar in the two anatomies, indicating the outer contour of the anatomy with average tissue properties throughout is a reasonable approach to estimating temperature rise while significantly lowering computational cost.Acknowledgements
The authors would like to thank FUJIFILM Healthcare Americas Corporation (Twinsburg, OH) for support of this project, for providing the RF coil model details, and providing access to and running the 1.2 T Hitachi Oasis open bore MRI system. The authors also would like to thank Siemens Healthineers (Erlangen, Germany) for providing information regarding their RF coils. The authors also thank AltaSim Technologies (Columbus, OH) for their help with the development and validation of the RF coil models in COMSOL Multiphysics®.References
1. ASTM F2503-20, Standard Practice for Marking Medical Devices and Other Items for Safety in the Magnetic Resonance Environment. ASTM International (2020).
2. Oasis 1.2T | Fujifilm Healthcare. https://hca.fujifilm.com/oasis-12t.
3. ASTM F2182-19E02, Standard Test Method for Measurement of Radio Frequency Induced Heating On or Near Passive Implants During Magnetic Resonance Imaging. ASTM International (2019).
4. Thermal Conductivity » IT’IS Foundation. https://itis.swiss/virtual-population/tissue-properties/database/thermal-conductivity/.
Figures