4770
Validation of Beat Sensor Cardiac Triggering against ECG Cardiac Triggering in both Volunteer and Patient Cohorts1Davis Heart and Lung Research Institute, The Ohio State University Wexner Medical Center, Columbus, OH, United States, 2Department of Biomedical Engineering, The Ohio State University, Columbus, OH, United States, 3Siemens Medical Solutions USA, Malvern, PA, United States, 4Siemens Healthcare GmbH, Erlangen, Germany, 5Department of Electrical and Computer Engineering, The Ohio State University, Columbus, OH, United States, 6Department of Internal Medicine, The Ohio State University Wexner Medical Center, Columbus, OH, United States
Synopsis
In this study, the performance of Beat Sensor Cardiac (BSC) triggering was qualitatively and quantitatively compared with electrocardiogram (ECG) triggering. MR images typically acquired in a comprehensive exam including localizer, morphology, cine, 2D flow, parametric mapping and late gadolinium enhancement (LGE) were acquired using both BSC and ECG triggering in volunteers and patients. The overall image quality for BSC was equivalent to ECG. Quantitative measurements of function, flow, and parametric maps in healthy volunteers showed no significant differences except for peak aortic velocity.
Introduction
ECG is the most commonly used triggering method for cardiac MRI. However, the patient preparation required to apply and adjust ECG electrodes can be time consuming. At higher field strengths, the ECG signal is prone to distortion due to gradient interference and the magnetohydrodynamic effect. BSC triggering is a Pilot Tone based method that does not require extra patient preparation. It utilizes an external radiofrequency (RF) signal that is modulated by the patient’s physiological motion1-3. In this study, we evaluated the performance of BSC vs. ECG triggering in a comprehensive cardiac MRI exam by comparing the quality of images and quantitative measurements.Methods
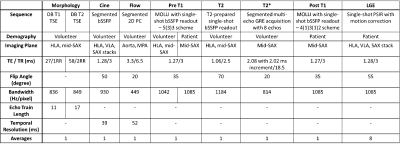
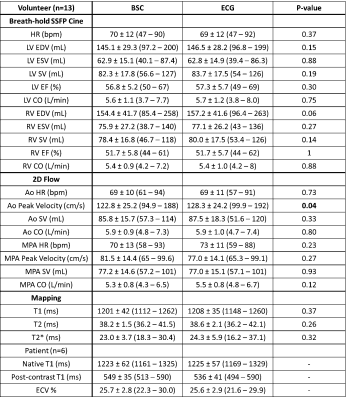
Both volunteer and patient data were collected with prototype sequences on a clinical 3T system (MAGETOM Vida, Siemens Healthcare, Erlangen, Germany). A calibration procedure was performed once at the beginning of the exam to train and calibrate BSC triggering signals and correct for signal interference caused by RF pulses. A comprehensive, non-contrast cardiac exam including localizer, morphology, cine, 2D flow, and parametric mapping was acquired in 14 volunteers (38 ± 14.5 years, 6 females) with both BSC and ECG triggering. Biventricular cardiac function and flow in aorta and main pulmonary artery (MPA, collected in 9 volunteers) were evaluated in suiteHEART (NeoSoft, Pewaukee, WI, USA). Myocardial T1, T2, and T2* values were measured in the interventricular septum. Pairwise student t-tests were performed to compare quantitative measurements from images acquired with BSC vs. ECG triggering.To evaluate the effectiveness of BSC triggering post contrast agent administration, BSC triggered pre- and post-contrast T1 maps and LGE were added to a standard ECG triggered clinical exam in 6 patients (27 ± 10.4 years, 4 females). Calibration was performed prior to contrast injection to evaluate the robustness of BSC triggering post-contrast. Scan parameters of BSC triggered sequences were set to match the ECG triggered clinical scans performed in the same patient. Inversion time (TI) in BSC triggered LGE scans were increased slightly relative to the ECG scans to account for the longer time after contrast injection. Pre- and post-contrast T1 maps were used to calculate extracellular volume (ECV). LGE image quality and sharpness were evaluated pairwise by a CMR expert (30 years of experience) blinded to the triggering method. Sequence types and corresponding imaging parameters for both volunteer and patient scans are shown in Table 1.
Results
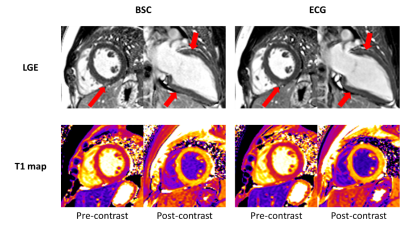
BSC triggered exams were successfully performed in all healthy volunteers and patients. All data from one volunteer were discarded due to gross patient motion observed between scans, resulting in poor correspondence of slice positions between BSC and ECG triggered images. Example images from healthy volunteers using both triggering methods are shown in Figure 1. All LGE images acquired in patients were reviewed and no significant differences in image quality or sharpness were detected. Figure 2 shows the LGE and T1 maps from one patient, showing mild enhancement in the basal to mid anterior and inferior wall in the long axis view, and at the RV attachment site in the mid short axis view. A summary of quantitative results measured in both volunteers and patients is shown in Table 2. Due to the limited size of the patient cohort, statistical analysis was performed in only healthy volunteers.Discussion
The feasibility of BSC triggering was evaluated by comparing with ECG triggering. The BSC utilizes an external RF signal to detect physiological motion. Depending on Pilot Tone transducer placement relative to the patient’s anatomy, the received signal characteristics can vary. Thus, a patient-specific training scan is required to calibrate the BSC trigger. Overall, nearly all comparisons demonstrated equivalent image quality and quantitative results. However, we did observe a systematic reduction in peak aortic velocity with BSC triggering. This could have been due to either a misalignment of image frames between ECG and BSC, or slight variations in BSC triggering between heartbeats. The triggering constancy relative to ECG needs further investigation. In Figure 2, signal to noise ratio in the blood pool appears slightly lower in the BSC triggered LGE and the post contrast T1 map. This could be due to the contrast agent washout from the blood pool because BSC triggered images were acquired later after contrast injection.Conclusion
Beat Sensor Cardiac triggered MR exam was successfully evaluated and validated in healthy volunteers and patients. Its performance was compared with standard ECG triggering across multiple imaging applications. The overall image quality was equivalent for BSC and ECG. Quantitative measurements in function, flow, and parametric maps in healthy volunteers showed no significant difference in all measurements except peak aortic velocity.Acknowledgements
Debbie Scandling, The Ohio State University, Columbus, OH, United States, for helping with volunteer recruitmentReferences
1. Schroeder, L., et al. A novel method for contact-free cardiac synchronization using the pilot tone navigator. in Proceedings of the 24th Annual Meeting of ISMRM, Singapore. 2016.
2. Bacher, M., Cardiac triggering based on locally generated pilot-tones in a commercial MRI scanner: a feasibility study. 2017.
3. Bacher M, Speier P, Bollenbeck J, Fenchel M, Stuber M: Pilot tone navigation enables contactless prospective cardiac triggering: initial volunteer results for prospective cine. In: Intl. Soc. Mag. Reson. Med, vol.26, p. 4798 (2018)
Figures