4701
Bone metastasis assessment using accelerated whole-body isotropic 3D T1-weighted Dixon acquisition with Compressed SENSE: a feasibility study1Department of Radiology, Deyang People's Hospital, Deyang, China, 2Philips Healthcare, Chengdu, China
Synopsis
Three-dimensional T1-weighted (T1W) Dixon as morphologic sequence has very high clinical value for the metastatic screening [1]. However, conventional multiplanar (CMP) T1W Dixon is limited by the long acquisition to achieve high resolution whole-body imaging. Therefore, this study aimed to achieve rapid whole-body high-resolution isotropic 3D T1W Dixon examination by Compressed SENSE (CSI T1W Dixon) and to investigate its feasibility in assessing bone metastases by comparing image quality and diagnosis performance with conventional multiplanar (CMP) (coronal, sagittal, axial planes) T1W Dixon scan. The results of this study suggested that high-resolution CSI T1W Dixon has potential to replace CMP T1W Dixon sequence for the assessment of bone metastasis in clinics with higher image quality and diagnostic capacity.
Introduction
Whole-body MRI has been well explored and has been proven successful to evaluate oncologic diseases in clinical practice , however, it is limited by long acquisition time due to multi-sequence and multi-planar imaging [2]. In recent years, fast-field-echo Dixon technique were commonly utilized to obtained T1W images because of its fast imaging speed than spin-echo imaging and allowing to generate four image types (in-phase, out-of-phase, water-only, and fat-only) in one-time acquisition. However, the Dixon technique is also limited by the long scan time to achieve high resolution whole-body imaging, which prevent its usage in daily clinical practice [2]. Recently, a combination of parallel imaging and compressed sensing (Compressed SENSE) has been developed to dramatically accelerate the acquisition while preserving high image quality [3]. The aim of this study was to achieve rapid whole-body high-resolution isotropic 3D T1W Dixon examination by Compressed SENSE (CSI T1W Dixon) and to investigate its feasibility in evaluating bone metastases in comparison with CMP (coronal, sagittal, axial) T1W Dixon scans.Materials and Methods
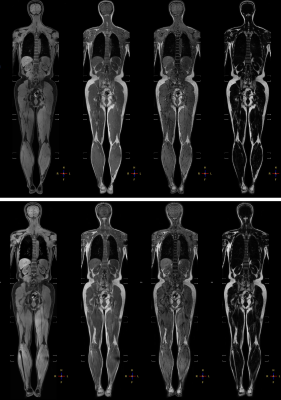
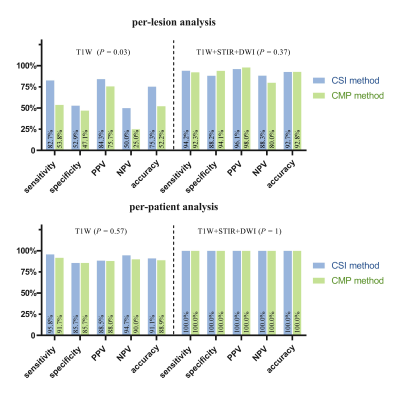
This study was approved by the institutional ethics committee. Forty-five consecutive patients with high-risk bone metastases were enrolled prospectively and underwent whole-body MRI on a 3T scanner with integrated 108 channels coils covering the whole body (Philips Healthcare, Ingenia, Netherlands). The sequences including high-resolution CSI T1W Dixon, three-plane (coronal, sagittal, axial) conventional T1W Dixon (CMP T1W Dixon), short tau inversion recovery (STIR), and difusion-weighted imaging (DWI). The optimized parameters for coronal CSI T1W Dixon included: scan time= 16.5 seconds; TR/TE1/TE2= 4.1 / 1.31 / 2.5 ms; FOV =380 × 398 × 350 mm3; acquisition voxel size =1.6 × 1.6 × 1.6 mm3; CS-SENSE factor= 7.6; water-fat shift= 0.4; flip angle= 10o; No. of signals acquired =1; No. of stations = 5; total acquisition time 83 seconds. Conventional T1W Dixon: scan time= 16.7 seconds; SENSE factor=2/2/2.8 for coronal/sagittal/axial, and the other parameters were aligned to be the same as CSI T1W Dixon. Conventional T1W Dixon scans were performed in coronal, sagittal and axial planes, with a total acquisition time of 251 seconds.The images of CSI T1 Dixon were reformatted into three-plane images of thick layers with identical geometry as the CMP T1 Dixon images. The reformatted CSI images and CMP images were graded by two radiologists with >10 years’ experience in whole-body MRI using a 4-point scale (1 = poor overall image quality / poor image clarity / severe artifacts, 2 = moderate overall image quality /moderate image clarity / moderate artifacts, 3 = good overall image quality/ good image clarity/ mild artifacts, 4 = excellent overall image quality/ excellent image clarity/ no artifacts with the evaluation indicators including overall image quality, image clarity, and severity of artifacts). Quantitative contrast-to-noise ratios (CNRs) between the spinal (or pelvic) metastases and their surrounding uninvolved bone tissues were calculated and compared for each type of Dixon images between reformatted CSI images and CMP images in coronal/sagittal/axial plane. In addition, the diagnostic performance (on per-lesion and per-patient) using T1 Dixon with/without combined STIR & DWI was compared between CSI and CMP methods. The combined biopsy and 6-month follow-up rescan imaging datasets were used as reference standards. Image quality scores and CNRs between the two methods were compared using Wilcoxon signed-rank test. The ROC analysis and Mcnemar test was applied to compare the diagnosis performance of per-patient analysis and per-lesion analysis, respectively. Statistical significance was defined as p < 0.05.
Results
Compared to conventional CMP Dixon acquisition, the scan time of with CSI Dixon acquisition was dramatically reduced (83 vs. 251 seconds). The scores between the reformatted CSI and CMP T1W Dixon images were found no significant difference for all the overall image quality and image clarity (p > 0.05). Whereas compared to CMP images, the reformatted CSI images observed significantly fewer artifacts (p < 0.05). In contrast to CMP T1W images, the images obtained by the CSI method had better CNR for each type of Dixon images in each plane (p = 0.001-0.02). Furthermore, the CSI T1W method provided a better diagnosis performance compared to the CMP method using the T1 Dixon without combined STIR & DWI evaluation for the per-lesion analysis (p = 0.03). While there was no significant difference in the diagnostic performance of T1 Dixon without combined STIR & DWI evaluation between the two methods. On the per-patient base, there was no significant difference between two T1 Dixon methods for both using T1 Dixon with/without combined STIR & DWI evaluation.Conclusion
The results of this study suggested that high-resolution CSI T1W Dixon, with shorter acquisition times, could yielded higher image quality and potentially higher diagnostic capacity compared with conventional CMP T1W Dixon. CSI T1W Dixon has potential to replace conventional multiplanar T1W Dixon sequence for the assessment of bone metastasis in clinics.Acknowledgements
NONEReferences
1. Lecouvet FE, Pasoglou V, Van Nieuwenhove S, Van Haver T, de Broqueville Q, Denolin V et al. Shortening the acquisition time of whole-body MRI: 3D T1 gradient echo Dixon vs fast spin echo for metastatic screening in prostate cancer. Eur Radiol. 2020;30(6):3083-93. doi:10.1007/s00330-019-06515-y.
2. Ma J, Costelloe CM, Madewell JE, Hortobagyi GN, Green MC, Cao G et al. Fast dixon-based multisequence and multiplanar MRI for whole-body detection of cancer metastases. J Magn Reson Imaging. 2009;29(5):1154-62. doi:10.1002/jmri.21746.
3. Nam JG, Lee JM, Lee SM, Kang HJ, Lee ES, Hur BY et al. High Acceleration Three-Dimensional T1-Weighted Dual Echo Dixon Hepatobiliary Phase Imaging Using Compressed Sensing-Sensitivity Encoding: Comparison of Image Quality and Solid Lesion Detectability with the Standard T1-Weighted Sequence. Korean J Radiol. 2019;20(3):438-48. doi:10.3348/kjr.2018.0310.
Figures