4667
Comparison of TGSE-BLADE, RESOLVE and SS-EPI for diffusion weighted imaging after cerebral aneurysmal clipping1Department of Diagnostic Imaging and Nuclear Medicine, Graduate School of Medicine, Kyoto University, Kyoto, Japan, 2Siemens Shenzhen Magnetic Resonance Ltd., Shenzhen, China
Synopsis
TGSE-BLADE DWI has been reported to reduce geometric distortion and susceptibility artifacts. However, it is unknown whether it reduces the clip-induced artifacts and improves image quality in patients after cerebral aneurysmal clipping. We compared the distortion and the artifacts between SS-EPI, RESOLVE, and TGSE-BLADE DWI in healthy volunteers and patients with a cerebral aneurysmal clip. TGSE-BLADE DWI has the best image quality regarding distortion and artifacts, especially at air-bone interfaces and near metal clips, which suggests that TGSE-BLADE DWI is a promising method for evaluating lesions at air-bone interfaces and scanning the patients with a clip.
Introduction
Echo-planar imaging (EPI) based diffusion-weighted imaging (DWI) techniques, e.g., SS-EPI and readout-segmented EPI (RESOLVE), are prone to susceptibility artifacts in the area where B0 field inhomogeneity presents, for example, near the air-bone interfaces and near metal clips. TGSE-BLADE DWI (The 2D turbo gradient- and spin-echo diffusion-weighted imaging with non-Cartesian BLADE trajectory) is insensitive to B0-related artifacts, leading to reduction of geometric distortion and susceptibility artifacts.1 There are a few reports about using TGSE-BLADE DWI2-4 to reduce geometric distortion and susceptibility artifact in regions where strong magnetic susceptibility presents. However, it is unknown whether TGSE-BLADE DWI is able to reduce the clip-induced artifacts and improves image quality in patients after cerebral aneurysmal clipping. The purpose of this study was to compare the distortion and the artifacts among three diffusion acquisition techniques (SS-EPI, RESOLVE, and TGSE-BLADE DWI) in healthy volunteers and patients with a cerebral aneurysmal clip.Methods
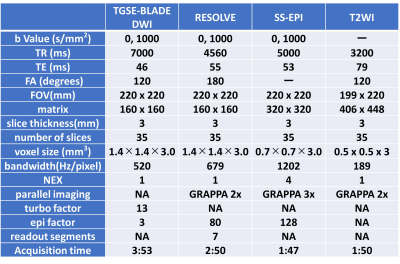
Subjects and Image AcquisitionSeventeen healthy volunteers (mean age 67.7, range 38-79 years) and eighteen patients who had undergone surgical cerebral aneurysmal clipping (mean age 66.9, range 40-86 years) were enrolled in this study under approval of institutional review board with written informed consent. The DWI sequences (SS-EPI, RESOLVE, and a prototype TGSE-BLADE DWI) and T2-weighted image (T2WI) for brain were performed at 3T MR scanners (MAGNETOM Skyra or MAGNETOM Prisma; Siemens Healthineers, Erlangen, Germany) with 32-channel head coil or 64-channel head/neck coil. The detailed imaging parameters are shown in Figure 1.
Image Analysis: healthy volunteers
The distortion was quantitatively examined for measuring the displacement between T2WI and each DWI sequence in the eight parts of brain: frontal lobes (near frontal sinus, anterior cranial base), parietal lobe, temporal tip, occipital lobe, pons, cerebellum near mastoid antrum and cerebellar hemisphere. Geometric distortion, susceptibility artifacts, overall image quality, and anatomic visualization of trigeminal nerve and vestibulocochlear nerve were assessed qualitatively using a 4-point Likert scale (1, poor; 2, fair; 3, good; 4, excellent).2
Image Analysis: patients after cerebral aneurysmal clipping
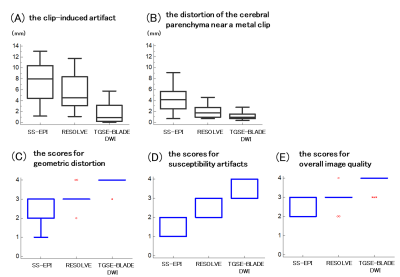
The length of the clip-induced artifact was measured on the images from T2WI and three DWI sequences, and the difference between T2WI and each DWI was calculated. The distortion of the cerebral parenchyma near a metal clip was evaluated for measuring the gap between T2WI and trace weighted images from each DWI sequence. Geometric distortion, susceptibility artifacts, and overall image quality were assessed qualitatively using a 4-point Likert scale.2
Statistical Analysis
The lengths and the scores were compared among the three DWI sequences using Friedman test and Wilcoxon signed-rank test with Bonferroni correction. A P value less than 0.017 was considered statistically significant.
Results
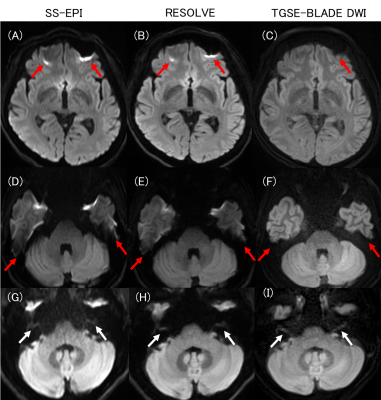
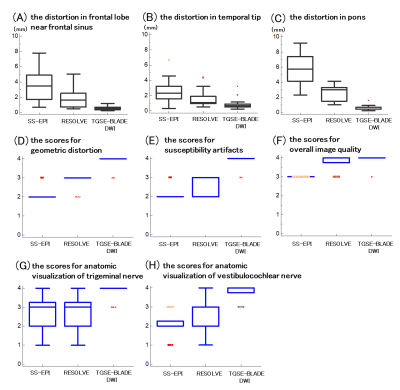
healthy volunteersThe distortion was the least significantly in TGSE-BLADE DWI, and statistically less in RESOLVE than in SS-EPI in two parts of frontal lobe, temporal tip, cerebellum near mastoid antrum and pons (P<0.001). The scores for geometric distortion and susceptibility artifacts were the best in TGSE-BLADE DWI, and better in RESOLVE than in SS-EPI (P<0.01). The score for overall image quality had no statistical difference between TGSE-BLADE DWI and RESOLVE, and the score in SS-EPI was worse than in RESOLVE and TGSE-BLADE DWI (P<0.001). The score for anatomic visualization of two nerves in TGSE-BLADE DWI was better than other two DWI sequences (P<0.001). RESOLVE and SS-EPI had no significant differences (Figure 2 and 3).
patients after cerebral aneurysmal clipping
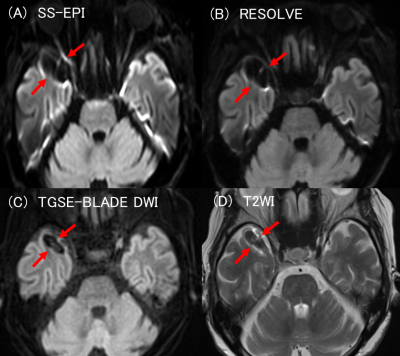
The length of the clip-induced artifact and the distortion of the cerebral parenchyma near a metal clip were the least significantly in TGSE-BLADE DWI, and statistically less in RESOLVE than in SS-EPI (P<0.01). The scores for geometric distortion, susceptibility artifacts and overall image quality were the best in TGSE-BLADE DWI, and better in RESOLVE than in SS-EPI (P<0.01) (Figure 4 and 5).
Discussion
The distortion was significantly the least near the air-bone interfaces (e.g., frontal lobe, temporal tip, cerebellum and pons) in TGSE-BLADE DWI. TGSE-BLADE DWI was also the best among the three DWI sequences in visualization of trigeminal nerve and vestibulocochlear nerve. These results suggest that TGSE-BLADE DWI is suitable for evaluating lesions near paranasal sinus, mastoid cells, and skull base, and at cranial nerves.Clip-induced artifact was the least in TGSE-BLADE DWI. The score for susceptibility artifacts was the best in TGSE-BLADE DWI.
Acute cerebral infarction often occurs after cerebral aneurysmal clipping, and TGSE-BLADE DWI seems to be useful for differentiating acute infarction and susceptibility artifact. For the score of overall image quality, TGSE-BLADE DWI and RESOLVE had no differences in healthy volunteers while TGSE-BLADE DWI was better than other DWI sequences in patients with aneurysmal clips. The result suggests that TGSE-BLADE is a promising DWI method for patients with clip, as it can provide better images and reduce artifacts comparing to other DWI methods.
Conclusion
TGSE-BLADE DWI has the best quality image regarding distortion and artifacts among the three DWI sequences in both healthy volunteers and patients who underwent aneurysmal clipping.Acknowledgements
We are grateful to Mr. Yuta Urushibata, Siemens Healthcare K. K., for his useful comments on this study.References
1. Hu HH, McAllister AS, Jin N, et al. Comparison of 2D BLADE Turbo Gradient- and Spin-Echo and 2D Spin-Echo Echo-Planar Diffusion-Weighted Brain MRI at 3 T: Preliminary Experience in Children. Acad Radiol 2019; 26(12): 1597-604.
2. Fu Q, Kong XC, Liu DX, et al. Clinical comparison of single-shot EPI, readout-segmented EPI and TGSE-BLADE for diffusion-weighted imaging of cerebellopontine angle tumors on 3 tesla. Magn Reson Imaging 2021; 84: 76-83.
3. Geng Y, Shi Y, Chen W, et al. BLADE turbo gradient- and spin-echo in the assessment of sinonasal lesions: a comprehensive comparison of image quality in readout-segmented echo-planar imaging. Acta Radiol 2021: 2841851211041820.
4. Sheng Y, Hong R, Sha Y, Zhang Z, Zhou K, Fu C. Performance of TGSE BLADE DWI compared with RESOLVE DWI in the diagnosis of cholesteatoma. BMC Med Imaging 2020; 20(1): 40.
Figures