4654
Distinction of compensated stage of liver cirrhosis in patients with chronic hepatitis B using IDEAL-IQ Magnetic Resonance Imaging1Radiology, Guangdong Hospital of Traditional Chinese Medicine, Zhuhai, China, 2MR Research, GE Healthcare, Beijing, China, 3Clinical Lab, Guangdong Hospital of Traditional Chinese Medicine, Zhuhai, China, 4Hepatology, Guangdong Hospital of Traditional Chinese Medicine, Zhuhai, China
Synopsis
The purpose was to evaluate the feasibility of IDEAL-IQ in distinction of patients with early liver cirrhosis(compensated stage). Sixty CHB patients with compensated cirrhosis conformed by liver biopsy and twenty healthy controls were recruited. FF and R2* of IDEAL-IQ sequence were analyzed between CHB compensated cirrhosis patients and volunteers. Correlations between FF and R2* and ALT, INR values were analyzed in CHB patients with compensated cirrhosis. R2* was statistically different between compensated cirrhosis patients and volunteers (p<0.01) with AUC of 0.726. The correlations between FF and ALT, INR were both fair(0.268, p=0.03 and -0.351, p<0.01).
Introduction
Approximately 3.5 billion patients suffer from chronic hepatitis B(CHB) worldwide and over 200,000 CHB patients die from cirrhosis each year1. It is known that cirrhosis could be reversed and adverse liver-related outcomes could be prevented by intervening with potent antiviral agents, oral anti-nucleotide drugs and/or interferon treatment2-6. Although liver biopsy has usually been required to confirm a diagnosis of liver cirrhosis, invasiveness and complications such as hemorrhage, infection are major issues7, 8. Thus, early and accurate non-invasive diagnosis of liver cirrhosis is important for clinicians to choose an appropriate treatment strategy for patients with CHB. Iterative Decomposition of water and fat with Echo Asymmetry and Least squares estimation(IDEAL-IQ) techniques based on magnetic resonance(MR) imaging have recently become widely used in nonalcoholic fatty liver disease(NAFLD), liver carcinoma, cancer patients under chemotherapy and living donor liver transplantation9-12. However, the utility of IDEAL-IQ has not yet been assessed in CHB cirrhosis patients. Our objective was to evaluate liver fat fraction(FF) and R2* values for the distinction of early cirrhosis(compensated stage) and to examine the potential correlation between FF, R2* and liver function in CHB patients with compensated cirrhosis.Methods
This prospective study was approved by the institutional ethical committee. Sixty CHB patients with early liver cirrhosis(compensated stage) conformed by liver biopsy and twenty healthy controls were recruited. All patients and volunteers underwent MR examinations including IDEAL-IQ sequence on 3.0T MR scanner. Three ROIs of 80-100mm2 were placed on the FF map and R2* map of segment VI(S6) of right liver while avoiding large vessels and bile ducts. Statistical analysis was performed using SPSS 26.0 software package. Hepatic FF and R2* obtained by using IDEAL-IQ sequence were calculated and compared using Mann-Whitney U test. Spearman correlations of measurements and ALT, INR were analyzed in patients. A 2-tailed p value <0.05 was considered statistically significant difference.Results
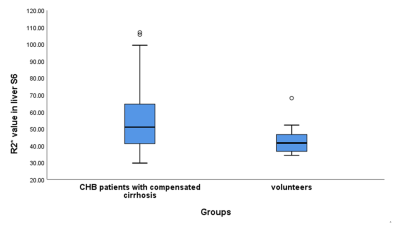
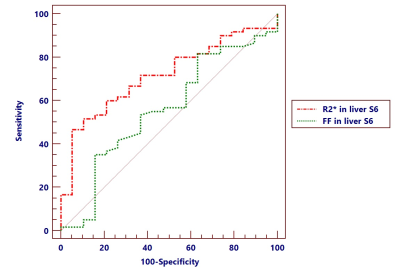
R2* value was statistically different between compensated cirrhosis patients and volunteers(Fig.1, 50.91 vs 41.90, p<0.01). ROC curves of R2* and FF were shown in Fig.2 and the AUC were 0.726 and 0.552, respectively. FF value was slightly higher in compensated cirrhosis patients than volunteers(2.99 vs 2.66, p=0.49). No correlation was found between R2* and ALT, INR. There was a positive fair correlation between liver FF and serum ALT(r=0.268, p=0.03) and a negative fair correlation with INR(r=-0.351, p<0.01).Discussion
Our study demonstrated that R2* was significantly higher in CHB patients with compensated cirrhosis than healthy controls. Chronic liver diseases is one of the reasons could cause secondary iron overload syndromes13. In cirrhosis patients, hepatocyte transferrin receptor proteins that mediate cellular iron uptake may be more active and result in selective iron accumulation14. Former original study also showed that hepatic iron overload was associated with a more severe stage of liver fibrosis among patients with chronic hepatitis C15. Measurements of ALT and INR activity is widely used for the diagnosis of liver cirrhosis in CHB patients. In our study, correlations between FF value and ALT, INR were both fair. Correlation between FF and ALT is consistent with previous study16. Thus, R2* value of IDEAL-IQ sequence was an alternative non-invasive method to distinguish CHB compensated cirrhosis patients from volunteers and liver FF value of IDEAL-IQ could reflect liver function in CHB patients with compensated cirrhosis.Conclusion
IDEAL-IQ has potential to detect early cirrhosis(compensated stage) in CHB patients as a non-invasive tool. There was a positive fair correlation between liver FF and serum ALT and a negative fair correlation between FF and INR levels.Acknowledgements
No acknowledgement found.References
1. Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ: Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. The Lancet 2015, 386(10003):1546-1555.
2. Yang YF, Zhao W, Zhong YD, Xia HM, Shen L, Zhang N: Interferon therapy in chronic hepatitis B reduces progression to cirrhosis and hepatocellular carcinoma: a meta-analysis. Journal of viral hepatitis 2009, 16(4):265-271.
3. Hadziyannis SJ, Tassopoulos NC, Heathcote EJ et al: Long-term therapy with adefovir dipivoxil for HBeAg-negative chronic hepatitis B for up to 5 years. Gastroenterology 2006, 131(6):1743-1751.
4. Dienstag JL, Goldin RD, Heathcote EJ et al: Histological outcome during long-term lamivudine therapy. Gastroenterology 2003, 124(1):105-117.
5. Su CW, Yang YY, Lin HC: Impact of etiological treatment on prognosis. Hepatology international 2018, 12(Suppl 1):56-67.
6. Buti M, Fung S, Gane E et al: Long-term clinical outcomes in cirrhotic chronic hepatitis B patients treated with tenofovir disoproxil fumarate for up to 5 years. Hepatology international 2015, 9(2):243-250.
7. Weigand K, Weigand K: Percutaneous liver biopsy: retrospective study over 15 years comparing 287 inpatients with 428 outpatients. Journal of gastroenterology and hepatology 2009, 24(5):792-799.
8. Bravo AA, Sheth SG, Chopra S: Liver biopsy. The New England journal of medicine 2001, 344(7):495-500.
9. Idilman IS, Aniktar H, Idilman R et al: Hepatic steatosis: quantification by proton density fat fraction with MR imaging versus liver biopsy. Radiology 2013, 267(3):767-775.
10. Chen R, Bai Y, Liu T et al: Evaluation of Glypican-3 Expression in Hepatocellular Carcinoma by Using IDEAL IQ Magnetic Resonance Imaging. Academic radiology 2021, 28(8):e227-e234.
11. Eskreis-Winkler S, Corrias G, Monti S et al: IDEAL-IQ in an oncologic population: meeting the challenge of concomitant liver fat and liver iron. Cancer Imaging 2018, 18(1):51.
12. Chiang HJ, Lin LH, Li CW et al: Magnetic resonance fat quantification in living donor liver transplantation. Transplantation proceedings 2014, 46(3):666-668.
13. Idilman IS, Akata D, Ozmen MN, Karcaaltincaba M: Different forms of iron accumulation in the liver on MRI. Diagnostic and interventional radiology 2016, 22(1):22-28.
14. Kadoya M, Matsui O, Kitagawa K et al: Segmental iron deposition in the liver due to decreased intrahepatic portal perfusion: findings at MR imaging. Radiology 1994, 193(3):671-676.
15. Souza RM, Freitas LA, Lyra AC, Moraes CF, Braga EL, Lyra LG: Effect of iron overload on the severity of liver histologic alterations and on the response to interferon and ribavirin therapy of patients with hepatitis C infection. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas 2006, 39(1):79-83.
16. Idilman IS, Tuzun A, Savas B et al: Quantification of liver, pancreas, kidney, and vertebral body MRI-PDFF in non-alcoholic fatty liver disease. Abdominal imaging 2015, 40(6):1512-1519.