4650
Intravoxel incoherent motion magnetic resonance imaging for the early detection of renal cold ischemia–reperfusion injury in a rat model1Tianjin First Central Hospital, Tianjin, China
Synopsis
The study evaluated the use of Intravoxel Incoherent Motion (IVIM) imaging to detect dynamic changes in renal microvascular characteristics during cold ischemia-reperfusion injuries (CIRIs). As previous studies have investigated warm ischemia-reperfusion injuries, we aimed to assess MR diffusion imaging in a renal CIRI Sprague Dawley rat model. Results showed that IVIM imaging is a sensitive tool to monitor changes in renal functional characteristics.
Introduction
Renal transplantation is an important treatment for end-stage renal diseases. Renal cold ischemia-reperfusion injury (CIRI) is one of the most serious complications following renal transplant[1,2]. The CIRI can increase the risk of acute renal injury, which may develop into chronic kidney disease, and even cause the delayed graft function (DGF), which seriously affects the quality of life of the patients and increases the rejection risk of the transplanted kidney[3,4]. The pathophysiological mechanism is complex and has not been fully revealed. CIRI consists of cold ischemia and reperfusion injury. However, CIRI is reversible in most cases, and therefore it is essential to monitor CIRI progression to improve treatment outcomes[5].Method
Forty-five rats were divided into the control group (N=5), the sham-operation group (N=20), and the CIRI group (N=20). Five rats were randomly selected, and IVIM images were acquired at one hour (1h), one day (1d), two days (2d), and five days (5d). The progressive changes in the diffusion (ADC, D) and perfusion (D*, f) parameters were studied in the renal cortex (CO), the outer stripe of the outer medulla (OSOM), and the inner stripe of the outer medullary (ISOM), followed by histological analysis to examine renal tubular injury scores and biochemical indicators to obtain the activity of superoxide dismutase (SOD). The two independent samples t-test was used to compare the differences in the measured parameters between the sham-operation group and the CIRI group at the same time. The one-way analysis of variance (ANOVA) and the least significant differences (LSD) tests were used to compare the measured parameters for different anatomical regions at different time points between the three groups. The Pearson correlation analysis was used to evaluate the correlation between the imaging parameters and the renal tubular injury scores and SOD levels.Results
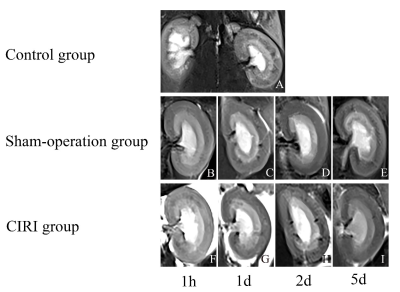
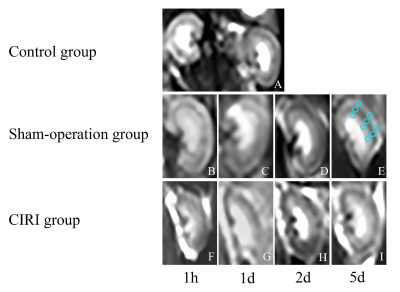
The T2WI and IVIM(b=0) images were shown in Figure 1. and Figure 2. The ADC and D values for all layers decreased at 1h (all P<0.05), then gradually increased back to the baseline at 5d. The D* value of all layers in the CIRI group transiently elevated at 1d (P<0.05), which was similar to the f values of OSOM and ISOM. The D* values within the OSOM were significantly different at 1h,1d, and 2d in the CIRI group (all P<0.05). The D* and f values of the OSOM and the ISOM layers at 5d were still significantly lower than the baseline (P<0.05) while the CO recovered (P>0.05). The f value of the OSOM was moderately negatively correlated with the renal tubular injury score in the CIRI and sham-operation groups (r = -0.464, P < 0.01) and moderately correlated with the SOD level in the CIRI group (r = -0.656, P < 0.01).Discussion
This study illustrated that IVIM parameters including ADC, D, D*, and f were significantly different with the development of renal CIRI in rat model. These findings indicate that multiparametric MRI is a permitted noninvasive, quantitative measurement reflective of water molecule diffusion and blood perfusion pertinent to the process of renal CIRI. From all investigated MRI parameters, the microcirculation measurements, D*, and f values provided more reliable information for detecting CIRI. Moreover, the f value of OSOM was correlated with the renal tubule injury score and SOD level. This demonstrates that the ratio of vascular and tubular fluid volume to the total fluid in OSOM reflected the pathophysiological progress effectively in CIRI.Conclusions
IVIM has excellent potential in monitoring renal CIRI progression. Measurements of microcirculation could provide more functional information about the kidneys following CIRI.Acknowledgements
The author(s) received the following financial support for the research, authorship, and/or publication of this article: This study was supported by grants from the National Natural Science Foundation of China (81873888).References
[1] Rabbat CG, Thorpe KE, Russell JD, Churchill DN. Comparison of mortality risk for dialysis patients and cadaveric first renal transplant recipients in Ontario, Canada. J Am Soc Nephrol 2000;11:917-22.
[2] Kootstra G, van Heurn E. Non-heartbeating donation of kidneys for transplantation. Nat Clin Pract Nephrol 2007;3:154-63. https://doi.org/10.1038/ncpneph0426.
[3] Hart A, Gustafson SK, Skeans MA, Stock P, Stewart D, Kasiske BL, et al. OPTN/SRTR 2015 Annual Data Report: Early effects of the new kidney allocation system. Am J Transplant 2017;17 Suppl 1:543-64. https://doi.org/10.1111/ajt.14132
[4] Zhang W, Zhao J, Cao F, Li S. Regulatory effect of immunosuppressive agents in mice with renal ischemia reperfusion injury. Exp Ther Med 2018;16:3584-8. https://doi.org/10.3892/etm.2018.6642.
[5] Francis A, Baynosa R. Ischaemia-reperfusion injury and hyperbaric oxygen pathways: a review of cellular mechanisms. Diving Hyperb Med 2017;47:110-7. https://doi.org/10.28920/dhm47.2.110-117.
Figures