4649
IVIM and DCE MRI to early detect hepatic injury and microcirculation alteration induced by intestinal ischemia reperfusion in a rat model1Radiology, The Affiliated ChangzhouNo.2 People's Hospital of Nanjing Medical University, Changzhou, China, 2MR Research China, Beijing, China, 3The Affiliated ChangzhouNo.2 People's Hospital of Nanjing Medical University, Changzhou, China
Synopsis
This study demonstrated that intravoxel incoherent motion (IVIM) and dynamic contrast enhanced (DCE) magnetic resonance imaging (MRI) can effectively estimate hepatic pathophysiological processes in a rat model with intestinal ischemia reperfusion (IIR) induced hepatic injury. The changes in microcirculation and perfusion were considered the major factors of IIR-induced hepatic injury. IVIM derived parameters of f and D* as well as DCE related parameter of Ve and Ktrans revealed high sensitivity to histological change, implying that IVIM and DCE-MRI might be an effective tool to evaluate the process of IIR-induced hepatic injury.
Introduction
Intestinal ischemia–reperfusion (IIR) injury is an irreversible and complex pathological process that occurs emergently in intestinal transplantation, hemorrhagic shock, intestinal volvulus, and intussusceptions.1 IIR not only injures viscera itself but also affects non-ischemic distant organs. In clinical practice, the diagnosis of hepatic injury is routinely based on the measurement of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) in serum. However, these indicators are only altered if substantial or potentially irreversible hepatic damage is present. Previous studies2 have shown that intravoxel incoherent motion (IVIM) with bi-exponential model enable water diffusion and perfusion measurement quantitatively to further evaluate hepatic injury. Meanwhile, dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI) was confirmed to be a valuable aid in the diagnosis and measurement of tissue perfusion and vascular permeability.3 With these promising results, combined IVIM and DCE-MRI however, have not been applied in hepatic injury induced by intestinal ischemia–reperfusion (IIR). Therefore, this study mainly aimed to examine whether IVIM and DCE-MRI can detect early IIR-induced hepatic changes, and to evaluate the separate relationships of IVIM and DCE-derived parameters with biochemical indicators and histological scores.Materials and Methods
Animal model Forty-two male Sprague–Dawley rats were randomly divided into the control group (Sham), the simple ischemia group, and the ischemia–reperfusion (IR) group (IR1h, IR2h, IR3h, and IR4h) in a rat model with secondary hepatic injury caused by IIR. IIR was induced by clamping the superior mesenteric artery for 60 minutes and then removing the vascular clamp. Histopathology was performed with hematoxylin and eosin staining. MRI experiment All MRI experiments were performed using a 3-T scanner (Discovery 750 W, GE Healthcare, USA). Spin-echo echo-planar imaging sequence (TR/TE = 3183/76 msec, slice thickness = 2 mm, FOV = 80 × 80 mm2, matrix = 160 × 160, 9 b-values = 20, 40, 60, 80, 100, 150, 200, 500, and 800 s/mm2) was applied for IVIM measurement. Fast spoiled gradient recalled-based sequence (TR/TE = 8.9/1.2 msec, slice thickness = 2 mm, acceleration factor = 2, FA = 12°, FOV = 90 × 55 mm2, matrix = 160 × 160, the time resolution was 8 s for a total of 45 time points) was used for DCE measurement. Data analysis All IVIM data was post-processed in vendor-provided software on GE Advanced Workstation (ADW4.6). DCE data was analyzed using OmniKinetics (OK) software. IVIM derived parameters, including apparent diffusion coefficient [ADC], true diffusion coefficient [D], perfusion-related diffusion [D*] and volume fraction [f], and DCE parameters of Ktrans, Kep, and Ve were obtained accordingly. All six regions of interest (ROI)s in the right lobe of liver were manually drawn on T2-weighted images (T2WI), and were then copied onto each functional parametric maps of IVIM and DCE. All ROIs were in the size of 6–8 mm2, and the mean value of six ROIs was calculated for the final data analysis. All statistic analyses were performed in SPSS 24.0 (Chicago, IL, USA) and GraphPad Prism 5.0 (San Diego, CA, USA). One-way analysis of variance (ANOVA) with Bonferroni post-hoc tests were used to measure the difference of the IVIM and DCE parameters and biochemical indicators among three different groups. Pearson correlation analysis was applied to determine the correlation between imaging parameters and biochemical indicators or histological score. P<0.05 was considered statistic significance.Results
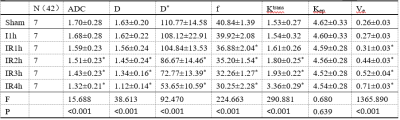
In all six groups, with extending reperfusion time, ADC, D, D*, and f gradually decreased, and Ktrans and Ve gradually increased (all P < 0.05, Table 1). In addition, Ktrans and Ve showed separate positive correlation with histological score, while each of ADC, D, f, and D* revealed negative correlations with histological score (all P < 0.05, FIGURE 1). For four IR subgroups, similar correlation relationships were also found between histological score and each of functional parameters (all P < 0.05, FIGURE 1).Discussion
In this study, we mainly investigated the feasibility of IVIM and DCE MRI in evaluating IIR-induced hepatic changes in a rat model. IVIM related results showed that ADC and D gradually decreased from the Sham group to the IR4h group, indicating that IIR can promote a progressive reduction in intrahepatic diffusion. Additionally, f and D* were gradually decreased from the Sham group to the IR4h group, demonstrating a decreased blood volume and the presence of microcirculatory disorder in the liver. For DCE, Ktrans value showed a gradual increase from the Sham group to the IR4h group, indicating the vascular permeability was increased. Also, Ve value gradually increased from the Sham group to the IR4h group, indicating an expansion of the extravascular extracellular space (EES) volume. Moreover, significant correlations were found between histological score and IVIM or DCE parameters in all six groups and in only four IR subgroups, which probably contributed to assessing the degree of damage in hepatic parenchyma.Conclusion
In conclusion, combined IVIM and DCE-MRI has demonstrated the potential of being an effective imaging tool in monitoring IIR-induced hepatic histopathology.Acknowledgements
No acknowledgement found.References
1. Zhao W, Gan X, Su G, et al. The interaction between oxidative stress and mast cell activation plays a role in acute lung injuries induced by intestinal ischemia-reperfusion. J Surg Res 2014; 187:542-552.
2. Wei Y, Gao F, Wang M, et al. Intravoxel incoherent motion diffusion-weighted imaging for assessment of histologic grade of hepatocellular carcinoma: Comparison of three methods for positioning region of interest. Eur Radiol 2019; 29:535-544.
3. Kim YS, Kim M, Choi SH, et al. Altered vascular permeability in migraine-associated brain regions: Evaluation with dynamic contrast-enhanced MRI. Radiology 2019; 292:713-720.
Figures