4637
Longitudinal Multiparametric Assessment of MRI in Symptomatic Knee Osteoarthritis and Correlation with Clinical Severity over 1 year1Korea University Guro Hospital, Seoul, Korea, Republic of, 2Siemens Healthcare, Seoul, Korea, Republic of
Synopsis
MRI is a valuable tool for to assess osteoarthritis (OA) progression. Although OA is a progressive degenerative disease involving the entire joint structure, cartilage degeneration is the central hallmark of the disease. MRI enables quantitative and semiquantitative assessment of longitudinal changes in articular cartilage morphology and composition in knee OA. We investigated the association between MRI biomarkers and knee OA progression over 12 months.
Body of the Abstract
PurposeTo assess the evolution of whole structural features, cartilage volume/thickness and prestructural features determined by knee MRI in patients with symptomatic OA over 1 year and to investigate their correlation with the change of clinical parameters.
Materials and Methods
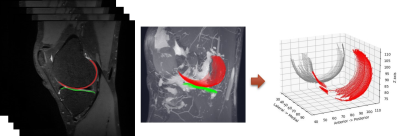
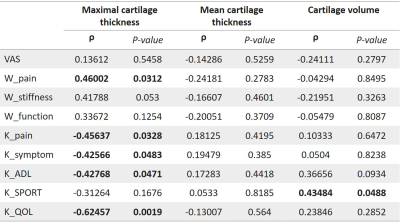
From December 2018 to May 2019, thirty patients with knee osteoarthritis were recruited. A total of 24 patients (13males, 11 females, mean age 67.0 years, range 42-79) completed the study. Patients were prospectively assessed at baseline and 1 year using clinical parameters as follows; visual analogue scale (VAS), Korean Western Ontario and McMaster Universities (KWOMAC), and Knee Injury Osteoarthritis Outcomes scores (KOOS). MRI was performed using 3D fat-suppressed proton density-weighted turbo spin echo (FS PD TSE), T1rho 3D and T2 map sequences, which were independently analyzed by two musculoskeletal radiologists (9 and 21 years of experience). Images were assessed using a whole-organ MRI scoring method (WORMS). T1rho and T2 values in cartilage at mid-sagittal image of medial femorotibial compartment (MFTJ) were measured. The cartilage of MFTJ were manually segmented from sagittal 3D FS PD TSE images using in-house developed software, and The cartilage thickness and volume of the segmented volumetric data were calculated. Spearman rank test was used to evaluate the association between the change of imaging findings and clinical parameters. Result The percentage of change of maximal cartilage thickness value in MFTJ were significantly correlated with that of WOMAC pain, positively, and KOOS pain, symptom, ADL and QOL, negatively. The percentage of change of WORMS cartilage score in MFTJ were significantly correlated with that of WOMAC function, positively. The percentage of change of WORMS cartilage score in total compartment had a positive significant correlation with WOMAC function, and negative significant correlation with KOOS pain. The percentage of change of subspinous bone marrow abnormality was correlated with that of KOOS pain, negatively. There was no significant association between T1 rho and T2 values of MFTJ cartilage and clinical parameters.
Discussion
Our study provides the longitudinal MRI assessment of cartilage change for OA progression. The change of semiquantitative cartilage scoring and cartilage thickness measured by MRI over 1 year were correlated with changes in clinical outcome parameters. Although bone marrow lesions, effusion-synovitis, and meniscal alterations were demonstrated as potential predictors for disease course in addition to cartilage, there were no significant association except for subspinous bone marrow edema in this study 1 -3. T1rho and T2 values are known to be able to detect early cartilage damage by reflecting the depletion of proteoglycan and collagen content in recent clinical trials 4. However, our results are not consistent with previous studies. We assumed that the clinical significance of T1 rho and T2 values for evaluating cartilage degeneration may be limited in advanced OA. There are several limitations in this study. First, this study had small sample size and heterogeneous population. Patients with severe OA as well as early OA were included. Second, T1rho and T2 values might be measured inappropriately owing to contamination of the cartilage signal by synovial fluid and misregistration related to different positions of 2D and 3D images. Third, cartilage thickness and volume were measured only in the MFTJ.
Conclusion
These results suggest that the change of maximal cartilage thickness and WORMS cartilage score of MFTJ, and subspinous bone marrow abnormality are significantly associated with clinical change in the symptomatic OA over I year.
Acknowledgements
None
References
1. Guermazi A, Roemer FW, Haugen IK, Crema MD, Hayashi D. MRI-based semiquantitative scoring of joint pathology in osteoarthritis. Nat Rev Rheumatol 2013;9:236–251.
2. Roemer FW, Guermazi A, Collins JE, et al. Semi-quantitative MRI biomarkers of knee osteoarthritis progression in the FNIH biomarkers consortium cohort - Methodologic aspects and definition of change. BMC Musculoskelet Disord 2016;17:466.
3. Shapiro LM, McWalter EJ, Son MS, Levenston M, Hargreaves BA, Gold GE. Mechanisms of osteoarthritis in the knee: MR imaging appearance. J Magn Reson Imaging. 2014;39:1346–1356.
4. Roemer FW, Demehri S, Omoumi P, et al. State of the Art: Imaging of Osteoarthritis–Revisited 2020. Radiology. 2020;296:5–21.
Figures