4632
Focused shape model assessment of cam-type femoroacetabular impingement: 3D MR cam morphology visualizations with associated surgical reviews1AEHRC, CSIRO, Brisbane, Australia, 2School of Information Technology and Electrical Engineering, University of Queensland, Brisbane, Australia, 3Institute of Bone and Joint Research, University of Sydney, Sydney, Australia, 4Department of Orthopaedic Surgery, John Hunter Hospital, Newcastle, Australia, 5Department of Rheumatology, Royal North Shore Hospital, St Leonards, Australia, 6School of Human Movement and Nutrition Sciences, University of Queensland, Brisbane, Australia
Synopsis
Evaluating hip shape change with statistical shape models (SSMs) has been reported as a biomarker for OA incidence, progression and end-stage outcomes. However, there have been few MR studies using 3D SSMs for assessing proximal femur shape, encompassing the femoral head-neck region, in patients with conditions such as FAI. To the best of our knowledge, we present the first study to use focused shape models from 3D MR hip images to assess a focal region of (clinical) interest for cam morphology evaluation in patients classified as having an ‘inadequate’, ‘borderline’ or ‘satisfactory’ surgical outcome as determined from expert surgical review.
Introduction
Cam-type femoroacetabular impingement (FAI) is a motion-related disorder causing hip and groin pain. In the general population, the prevalence of cam morphology is 15 - 25 % in males and 5 - 15 % in females1-3 and has been reported to account for 37% of the morphologies in FAI syndrome 4. There has been a series of studies that support a strong association between increased cam size and the development of hip osteoarthritis (OA) 5-10. Although the evaluation of hip bone shape change with statistical shape models (SSMs) has been reported as a biomarker for hip OA incidence, progression and end-stage outcomes in radiographic studies 11-13, there have been few magnetic resonance (MR) SSM-based studies for bone shape assessment of the proximal head-neck region of the femur 14,15. This current study is the first to use a novel automated segmentation framework (CamMorph) to assess pre- and post-operative focused shape modelling (FSM) results for individual cases classified with surgical outcomes by an expert surgeon panel.Methods
CamMorph was used to segment and assess MR images of the hip joint from the Australian FASHIoN trial 16, a multi-centre randomised controlled trial that assessed hip cartilage health 17 in FAI-syndrome patients treated with physiotherapist-led intervention or hip arthroscopy 16. Overall, 97 patients (56M, 41F, aged 16 – 63 years) were assessed. The MR examinations analysed within the current study were acquired using a sagittal three-dimensional (3D) T2-weighted true fast imaging with steady-state precession sequence (TR: 10.2ms,TE: 4.3ms, image spacing: 0.644 x 0.644 x 0.668, FOV: 16 x 16 cm, matrix: 256 x 256). Briefly, CamMorph generates an initial proximal femur bone segmentation using a 3D U-net based and FSM approach. Subsequently, patient-specific anatomical information from the FSM is used to simulate ‘healthy’ 3D femoral bone models and pathological region constraints for cam morphology identification. Here, pre- and post-operative 3D FSMs (incorporating a “heat” map for cam height) from representative arthroscopic patients were chosen for visualization 18 and observational evaluations with a priori reports of surgical outcomes from expert surgical assessments. The patients included for the current analyses included 1 patient classified with an ‘inadequate’ post-surgical outcome, 1 patient classified with a ‘borderline’ post-surgical outcome and 1 patient classified with a ‘satisfactory’ surgical outcome.Results
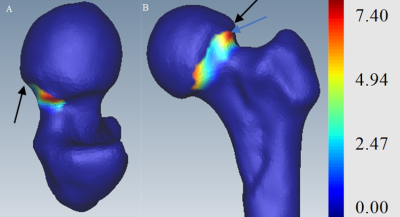
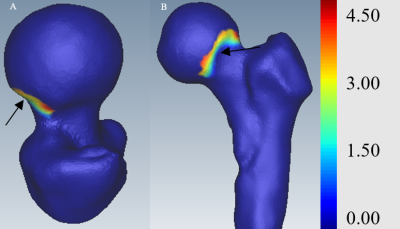
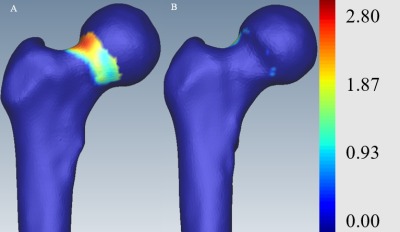
Figure 1 shows post-operative 3D FSMs for Case 1 in which the expert surgical assessment indicated there was an ‘inadequate’ surgical outcome. Specifically, the expert surgical review stated the patient had an “aspherical head at 12 and 3 (o’clock) with sharp transition at 12 (o’clock)”. The post-operative 3D FSMs are shown for Case 2 (Figure 2), where the expert assessment reported a ‘borderline’ surgical outcome with a description of “dysplastic hip, femoral head shape ok”. The pre- and post-operative 3D FSMs for Case 3, a patient described as having a ‘satisfactory’ surgical outcome, provide a clear-cut visualization of cam bone mass removal arising from ostectomy (Figure 3). The expert surgical review stated that this patient had a “good reshaping” of the femoral head following the arthroscopic procedure.Discussion
There was good concordance between the 3D FSM visualizations of cam morphology / height data / femur bone shape and the a priori reports of expert surgical assessments based on pre- and post-operative MR imaging, intra-operative arthroscopic images and operative reports. Visualization of the 3D FSMs across a spectrum of FAI cases with expert surgical outcome evaluations ranging from ‘inadequate’, ‘borderline’ and ‘satisfactory’ clearly showed post-operative features such as asphericity of the femoral head and sharp transitions (‘inadequate’ outcome), an “okay” post-ostectomy femoral head shape (‘borderline’ outcome) in a patient with cam morphology in conjunction with a dysplastic hip joint and essentially complete removal of cam bone mass, assessed following post-arthroscopic treatment, in a patient reported to have a ‘satisfactory’ surgical outcome.Conclusion
The cam-related FAI cases analysed within this work suggest that 3D FSM-based cam morphology assessments were consistent with post-operative outcome reviews made by an expert surgical panel to classify patients with an ‘inadequate’, ‘borderline’ or ‘satisfactory’ surgical outcome. Future work is needed to assess the potential clinical utility of 3D FSM-based cam morphology assessment in aspects such as treatment decisions, pre-surgical and post-surgical evaluations.Acknowledgements
No acknowledgement found.References
1. Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of Malformations of the Hip Joint and Their Relationship to Sex, Groin Pain, and Risk of Osteoarthritis: A Population-Based Survey. J Bone Joint Surg Am. 2010;92(5):1162-1169.
2. Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of Cam-Type Femoroacetabular Impingement Morphology in Asymptomatic Volunteers. J Bone Joint Surg Am. 2010;92(14):2436-2444.
3. Reichenbach S, Jüni P, Werlen S, et al. Prevalence of cam‐type deformity on hip magnetic resonance imaging in young males: A cross‐sectional study. Arthritis Care Res (Hoboken). 2010;62(9):1319-1327.
4. Frank JM, Harris JD, Erickson BJ, et al. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2015;31(6):1199-1204.
5. Agricola R, Waarsing JH, Arden NK, et al. Cam impingement of the hip—a risk factor for hip osteoarthritis. Nature Reviews Rheumatology. 2013;9(10):630-634.
6. Saberi Hosnijeh F, Zuiderwijk ME, Versteeg M, et al. Cam Deformity and Acetabular Dysplasia as Risk Factors for Hip Osteoarthritis. Arthritis & Rheumatology. 2017;69(1):86-93.
7. Klij Pv, Heerey J, Waarsing JH, Agricola R. The Prevalence of Cam and Pincer Morphology and Its Association With Development of Hip Osteoarthritis. Journal of Orthopaedic & Sports Physical Therapy. 2018;48(4):230-238.
8. Kemp JL, Crossley KM, Agricola R, Geuskens F, van Middelkoop M. Radiographic hip osteoarthritis is prevalent, and is related to cam deformity 12-24 months post-hip arthroscopy. International journal of sports physical therapy. 2018;13(2):177.
9. Zeng W-N, Wang F-Y, Chen C, et al. Investigation of association between hip morphology and prevalence of osteoarthritis. Scientific Reports. 2016;6(1):23477.
10. Nelson AE. The Importance of Hip Shape in Predicting Hip Osteoarthritis. Current Treatment Options in Rheumatology. 2018;4(2):214-222.
11. Gregory JS, Waarsing JH, Day J, et al. Early identification of radiographic osteoarthritis of the hip using an active shape model to quantify changes in bone morphometric features: Can hip shape tell us anything about the progression of osteoarthritis? Arthritis & Rheumatism. 2007;56(11):3634-3643.
12. Barr RJ, Gregory JS, Reid DM, et al. Predicting OA progression to total hip replacement: can we do better than risk factors alone using active shape modelling as an imaging biomarker? Rheumatology. 2011;51(3):562-570.
13. Castaño-Betancourt MC, Van Meurs JBJ, Bierma-Zeinstra S, et al. The contribution of hip geometry to the prediction of hip osteoarthritis. Osteoarthritis and Cartilage. 2013;21(10):1530-1536.
14. Schmid J, Kim J, Magnenat-Thalmann N. Robust statistical shape models for MRI bone segmentation in presence of small field of view. Medical image analysis. 2011;15(1):155-168.
15. Chandra SS, Xia Y, Engstrom C, Crozier S, Schwarz R, Fripp J. Focused shape models for hip joint segmentation in 3D magnetic resonance images. Medical Image Analysis. 2014;18(3):12.
16. Murphy NJ, Eyles J, Bennell KL, et al. Protocol for a multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapy-led care for femoroacetabular impingement (FAI): the Australian FASHIoN trial. BMC Musculoskeletal Disorders. 2017;18(1):406.
17. Mamisch TC, Kain MSH, Bittersohl B, et al. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC) in Femoacetabular impingement. Journal of Orthopaedic Research. 2011;29(9):1305-1311.
18. Chandra SS, Dowling JA, Engstrom C, et al. A lightweight rapid application development framework for biomedical image analysis. Computer Methods and Programs in Biomedicine. 2018;164:193-205.
Figures