4601
High-resolution compressed sensing TOF-MRA might show better performance than CTA for evaluating revascularization in Moyamoya patients1Department of Radiology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2Department of Neurosurgery, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 3Siemens Healthcare, Erlangen, Germany, 4Siemens Healthcare, Shanghai, China
Synopsis
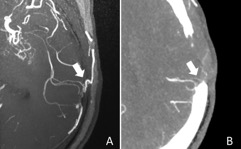
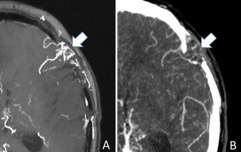
It is important for MMD patients to receive repeated life-time follow-up examinations for evaluation of bypass patency and collateral formation from neovascularization after bypass surgery. In this study we evaluated the clinical value of high-resolution (0.4 × 0.4 × 0.4 mm3 isotropic) CS TOF-MRA for assessment of STA-MCA bypass and neovascularization by using CTA as the reference. We found that high-resolution CS TOF-MRA could provide better visualization for both STA-MCA bypass and neovascularization than traditional CTA within a clinically reasonable time in MMD patients after surgical revascularization.
Introduction and Purpose
Moyamoya disease (MMD) is a progressive steno-occlusive disease at terminal portions of the internal carotid arteries, which leads to an abnormal vascular network at the base of the brain1. Direct revascularization such as anastomosis of the superficial temporal artery (STA) and middle cerebral artery (MCA) combined with indirect revascularization is an effective procedure for MMD patients2. Long-term evaluation of bypass patency and collateral formation from neovascularization after bypass surgery is extremely important for MMD patients. DSA has long been the gold standard for assessing the patency of the STA-MCA anastomosis postoperatively, but it is an invasive, radiation-associated technique with the possibility of complications. CTA is the most commonly used technique to evaluate and follow up patients with STA-MCA bypass. However, CTA suffers from several disadvantages including the need for contrast medium, radiation exposure and interference from the skull. Conventional TOF-MRA can be repeatedly used for follow-up examinations, especially benefit for pediatric patients. However, it has limitations in the visualization of small and distal arterial branches. Compressed sensing (CS) allows rapid acquisition of images by using fewer k-space samples3. Furthermore, CS TOF-MRA may have advantage in displaying small and distal vessels4. Thus, we aimed to evaluate the utility of CS TOF-MRA for assessment of revascularization by comparison with CTA.Methods
Twenty moyamoya patients after surgical revascularizations who underwent CS TOF-MRA and CTA were collected. CS TOF-MRA was performed based on a research sequence and reconstruction prototype on a MAGNETOM Skyra 3T MR scanner (Siemens Healthcare, Erlangen, Germany) with a 20-channel head/neck coil. The slice orientation was axial. The parameters were as follows: TR 21 ms, TE 3.49 ms, flip angle 18°, FOV 220 × 200 mm2, matrix 368 × 334, slice thickness 0.4 mm, and number of slabs 4. The acquired voxel size was 0.6 × 0.6 × 0.6 mm3 and reconstructed to 0.4 × 0.4 × 0.4 mm3, and the acceleration factor of CS TOF-MRA was set at 5. Neither phase nor slice partial Fourier was used. The scan range extended from C5 of the ICA to M4 of the MCA, covering both the STA-MCA bypass and the circle of Willis. The total acquisition time was 5 minutes and 4 seconds. Data were reconstructed using 10 iterations of the modified fast iterative shrinkage-thresholding algorithm. The reconstruction time was one minute and 18 seconds.MIP images and source images of CS TOF-MRA and CTA were both used for imaging evaluation. Images were assessed independently in a randomized order by two neuroradiologists. Visualization of STA and MCA bypass, and neovascularization into the brain pial surface were ranked based on a 4-point scale respectively on CS TOF-MRA and CTA5, 6. The patency of anastomosis was assessed as open or closed7. Interobserver agreement was calculated using the weighted kappa statistic. Wilcoxon signed-rank or Chi-square test was performed to investigate diagnostic difference between CS TOF-MRA and CTA.
Results
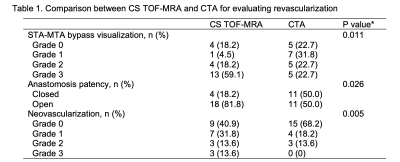
Twenty-two hemispheres from 20 patients were analyzed. The interrater agreement for evaluating STA-MCA bypass, neovascularization and anastomosis patency was good to excellent (κCS TOF-MRA, 0.738-1.000; κCTA, 0.743-0.909). The diagnostic grade of bypass visualization on CS TOF-MRA (59.1% of grade 3) were significantly higher than that of CTA (22.7% of grade 3) (P = 0.011). More anastomoses were found open on CS TOF-MRA (81.8%) than CTA (50.0%) (P = 0.026). Neovascularization was better observed in 13 (59.1%) sides on CS TOF-MRA, in comparison to 7 (31.8%) sides on CTA images (P = 0.005).Discussion
In this current study, the scan time of CS TOF-MRA for achieving a high-resolution spatial resolution (0.4 × 0.4 × 0.4 mm3) was 5 minutes and 4 seconds. This compares favorably to a conventional TOF-MRA with parallel imaging (GRAPPA 2, phase and slice partial Fourier, 7/8) which takes 10 minutes and 8 seconds using equivalent resolution and coverage to CS TOF-MRA. Therefore, the acquisition time was significantly reduced. And our results indicated that CS TOF-MRA with an acceleration factor of 5 could provide sufficient diagnostic quality and more clear visualization of STA-MCA bypass and neovascularization than traditional CTA while keeping a clinically reasonable scan time.Several advantages make CS TOF-MRA possible to better depict the bypass and neovascularization than traditional CTA. First, TOF-MRA is based on the principle of flow-related enhancement, which highlights the vessel signal and suppresses the background signal. By combining TOF-MRA and CS, the image quality of CS TOF-MRA gets better by enhancing the contrast of vessels due to inherently denoising procedure of CS reconstruction8. Second, the high-resolution spatial resolution of CS TOF-MRA was isotropic (0.4 × 0.4 × 0.4 mm3), which was convenient to reconstruct and better display the bypass. Moreover, in addition to traditional advantages such as radiation free, no need for contrast medium and simply be run by technologists, CS TOF-MRA can be performed in combination with other MR sequences, which can sensitively depict changes in the brain parenchyma following surgery. In contrast, CTA has several limitations including interference from background increased signals and skull.
Conclusion
High-resolution CS TOF-MRA might perform better than CTA for visualization of both STA-MCA bypass and neovascularization within a clinically reasonable time in Moyamoya patients after revascularization.Acknowledgements
We sincerely thank the participants in this study.References
1.Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo)2012;52:245-266
2.Acker G, Fekonja L, Vajkoczy P. Surgical Management of Moyamoya Disease. Stroke 2018;49:476-482
3.Hollingsworth KG. Reducing acquisition time in clinical MRI by data undersampling and compressed sensing reconstruction. Phys Med Biol 2015;60:R297-322
4.Lin Z, Zhang X, Guo L, et al. Clinical feasibility study of 3D intracranial magnetic resonance angiography using compressed sensing. J Magn Reson Imaging 2019;50:1843-1851
5.Tang H, Hu N, Yuan Y, et al. Accelerated Time-of-Flight Magnetic Resonance Angiography with Sparse Undersampling and Iterative Reconstruction for the Evaluation of Intracranial Arteries. Korean J Radiol 2019;20:265-274
6.Zhao Y, Li J, Lu J, et al. Predictors of neoangiogenesis after indirect revascularization in moyamoya disease: a multicenter retrospective study. J Neurosurg 2019:1-11
7.Wang M, Yang Y, Wang Y, et al. Vessel-selective 4D MRA based on ASL might potentially show better performance than 3D TOF MRA for treatment evaluation in patients with intra-extracranial bypass surgery: a prospective study. Eur Radiol 2021;31:5263-5271
8.Yamamoto T, Okada T, Fushimi Y, et al. Magnetic resonance angiography with compressed sensing: An evaluation of moyamoya disease. PLoS One 2018;13:e0189493
Figures