4592
Arterial transit artifact could prognose stroke patients beyond 24 hours from last known well1Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China, 2Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China, 3GE Healthcare, Beijing, China, Beijing, China, 4Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Synopsis
The study aimed to assess the correlation of arterial transit artifact (ATA) with clinical outcomes and collateral circulation status in stroke patients beyond 24 hours from last known well. ATA is assessed by 3-dimentional pseudo-continuous ASL (3D-pCASL), collateral status by magnetic resonance angiography (MRA) using a grading system from 0 to 3, and clinical outcomes by 3-month modified Ranking Scale (3m-mRS). ATA was present in about half of the enrolled patients, most of whom had large artery disease. Though the correlation between ATA and the degree of collateral supply was not statistically significant, ATA could predict the favorable clinical outcomes.
Introduction
The extent of collateral flow and the degree of reperfusion play a major role in the outcome of ischemic stroke. 1 Collaterals can be quantified with angiographic methods, such as MRA, CTA and DSA. On ASL images, the collaterals can also be identified as a focus or serpiginous hyperintensity that was located bordering the region of perfusion defects 2, known as ATA. ATA has been found correlated with tissue survival and improved clinical outcome in acute ischemic patients 2, 3. However, there is still dearth of data regarding ATA in stroke patients beyond 24 hours from last known well who lost the opportunity to receive an endovascular therapy but still have salvageable brain tissue4. Besides, little work has been done to uncover the relationship between ATA status and quantitative collateral circulation. We preliminarily focused on the population beyond the endovascular therapeutic time window and aimed to assess the correlation of ATA with clinical outcomes and collateral circulation score using time-of-flight MRA (TOF-MRA).Materials and methods
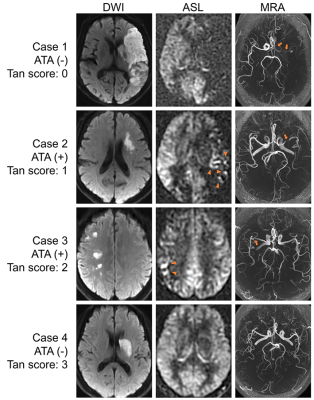
This study was approved by the ethics committee of local institution. Patients admitted to our hospital with first-ever unilateral anterior circulation ischemic stroke were enrolled. Clinical severity was evaluated using National Institutes of Health Stroke Scale on admission (baseline-NIHSS). Primary clinical outcome was 3m-mRS score either by telephone or clinical visit and the second outcome was functional independence (FI, 3m-mRS ≤ 2) or functional dependence (FD, 3m-mRS > 2). Diffusion-weighted imaging (DWI), conventional T1-/T2- weighted imaging, 3D-pCASL and TOF-MRA were scanned on a 3.0 Tesla MRI scanner (Discovery MR750, GE Healthcare) with a 32-channel head coil. Apparent diffusion coefficient (ADC, × 10-6 mm2/s) maps were generated automatically from the DWI data on GE workstation. A threshold of 620 × 10-6 mm2/s was set to calculate the infarct volume 5. ATA was defined as serpiginous hyperintensity or a focus overlying the bordering of perfusion defects on the original images of 3D-pCASL 2. The offending arteries were dichotomized into major intracranial arteries (carotid, middle cerebral, anterior cerebral) and small vessels (lenticulostriate, anterior choroidal artery) according to the lesion location on DWIs and vessel status on TOF-MRA. The percent stenosis of the major intracranial arteries was measured using WASID method 6. The collaterals filling on TOF-MRA were scored from 0 to 3 according to the grading system proposed by Tan et al 7. Statistical analyses were carried out using IBM SPSS Statistics 26 (Armonk, NY, USA).Results
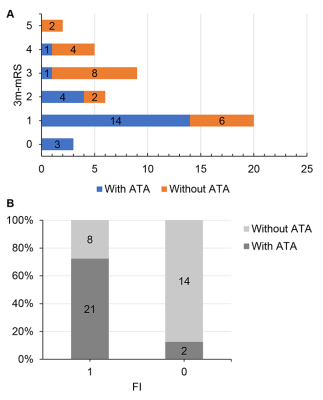
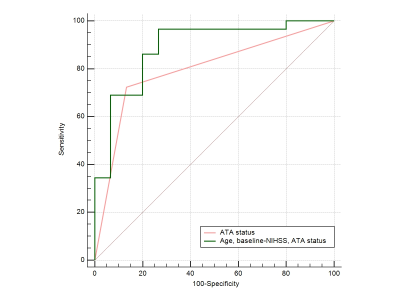
A total of 45 patients were included (age, 55 ± 10 years; male, 36 [80.0%]). The time interval (TI) from stroke symptom onset to MRI was 75.1 ± 31.4 hours. ATAs were present in 23 (51.1%) patients (Figure 1). Patients with ATA showed less severe manifestation according to baseline-NIHSS (P = 0.014) and better 3-month clinical outcome (P < 0.001) compared to patients without ATA (Table 1; Figure 2). FI recovered in twenty-one (91.3%) of patients while in only 8 (36.4%) without ATA (P < 0.001). There were no significant differences of age, sex, risk factors, lesion volume and TI between two groups. Meanwhile, ATA was significantly correlated with large artery stenosis (P < 0.001) but not with the stenotic degree (P = 0.717). Of the patients with large artery stenosis (28, 62.2%), there was no significant correlation of ATA and collateral score (P > 0.05; data not shown). Finally, age, baseline NIHSS, and status of ATA were selected into a binary logistic regression model for prediction of secondary clinical outcome (χ2 = 21.732, P < 0.001). However, only the status of ATA was statistically significant (OR = 15.213, 95% CI: 2.376-97.396). The model could predict the clinical outcome at the AUC of 0.887 with sensitivity being 96.55% and specificity 73.33% (Figure 3).Discussion
In this study, we explored the relationship between ATA and clinical outcome and collateral circulation score of ischemic stroke patients beyond 24 hours from last known well. Patients could benefit from ATA when missing the best therapeutic window, showing less severe manifestation on admission and better 3-month prognosis. Previous studies have attempted uncovering the benefit of good collateral perfusion to neurological improvement 3, 8. ATA, derived from the sensitivity of ASL of the delayed arterial arrivals, can reflect slow retrograde collateral circulation which compensates the lack of anterograde flow 9, 10. Okazaki et al. 3 reported the emergence of ATA during thrombolysis by repeated ASL and its ability to predict complete reperfusion, early neurological recovery and stable infarct after thrombolysis. Havenon et al. 2 found strong association between the ASL collaterals and better outcome at hospital discharge. Our results further proved that ATA sustains a positive effect on ischemic patients beyond 24 hours from last known well. No correlation between ATA and collateral score suggested that ATA captures extra information besides the collateral flow measured by angiographic methods. Since a study from DEFUSE 3 reported there is a link between persistent penumbral beyond 24 hours and poor prognosis 4, ATA may serve as a useful imaging biomarker to identify the status of collateral circulation and guide the therapeutic strategies for late window patients.Acknowledgements
Funding: This project was supported by the National Natural Science Funds of China (Grants No.81801666, 81570462 and 81730049).References
1. Cipolla MJ. Thomas Willis Lecture: Targeting Brain Arterioles for Acute Stroke Treatment. Stroke. 2021; 52: 2465-77.
2. de Havenon A, Haynor DR, Tirschwell DL, et al. Association of Collateral Blood Vessels Detected by Arterial Spin Labeling Magnetic Resonance Imaging With Neurological Outcome After Ischemic Stroke. JAMA neurology. 2017; 74: 453-8.
3. Okazaki S, Griebe M, Gregori J, et al. Prediction of Early Reperfusion From Repeated Arterial Spin Labeling Perfusion Magnetic Resonance Imaging During Intravenous Thrombolysis. Stroke. 2016; 47: 247-50.
4. Sarraj A, Mlynash M, Heit J, et al. Clinical Outcomes and Identification of Patients With Persistent Penumbral Profiles Beyond 24 Hours From Last Known Well: Analysis From DEFUSE 3. Stroke. 2021; 52: 838-49.
5. Purushotham A, Campbell BC, Straka M, et al. Apparent diffusion coefficient threshold for delineation of ischemic core. International journal of stroke : official journal of the International Stroke Society. 2015; 10: 348-53.
6. Samuels OB, Joseph GJ, Lynn MJ, Smith HA and Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR American journal of neuroradiology. 2000; 21: 643-6.
7. Tan IY, Demchuk AM, Hopyan J, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR American journal of neuroradiology. 2009; 30: 525-31.
8. Flores A, Rubiera M, Ribo M, et al. Poor Collateral Circulation Assessed by Multiphase Computed Tomographic Angiography Predicts Malignant Middle Cerebral Artery Evolution After Reperfusion Therapies. Stroke. 2015; 46: 3149-53.
9. Chalela JA, Alsop DC, Gonzalez-Atavales JB, Maldjian JA, Kasner SE and Detre JA. Magnetic resonance perfusion imaging in acute ischemic stroke using continuous arterial spin labeling. Stroke. 2000; 31: 680-7.
10. Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME and Steinberg GK. Arterial Spin-Labeling MRI Can Identify the Presence and Intensity of Collateral Perfusion in Patients With Moyamoya Disease. Stroke. 2011; 42: 2485-U183.
Figures