4588
High prediction accuracy for functional outcome of acute ischemic stroke using nomogram based on clinical factors and radiomics features1Tongji Hospital affiliated to Tongji Medical College of Huazhong University of Science & Technology, Wuhan, China, 2GE Healthcare, Beijing, China
Synopsis
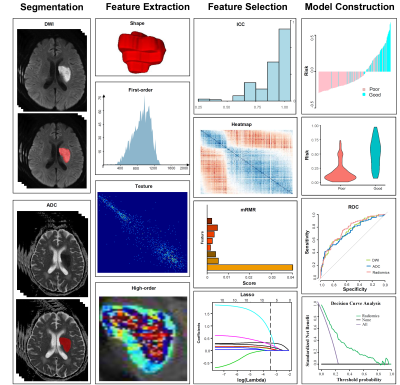
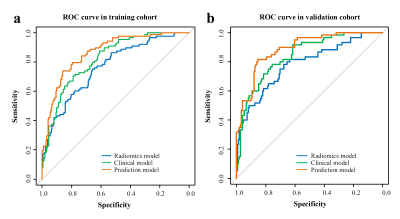
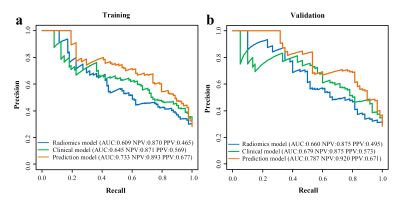
To develop a nomogram for accurate prediction of acute ischemic stroke (AIS) outcome, 522 AIS patients were retrospectively selected in this study. Radiomics features were extracted from DWI and ADC maps and radiomics score was established. Logistic regression analysis was implemented to sift independent clinical factors and construct prediction model. Finally, the nomogram incorporated age, sex, stroke history, diabetes, baseline modified Rankin Scale, baseline National Institutes of Health Stroke Scale score and radiomics score yield the great predictive performance with an AUC-ROC of 0.868 in training cohort and 0.890 in validation cohort, the AUC-PR reached 0.733 and 0.787 respectively.
Introduction
Stroke is the second leading cause of death and the third leading cause of disability in global [1]. Accurate prediction for patient outcome would help clinicians understand patient conditions at the early onset stage and make an individualized treatment plan [2]. Radiomics as an emerging methodology has been used to study tumor grading and type, tumor heterogeneity, and survival of glioma patients with excellent results [3, 4]. Moreover, radiomics features of MR images have been shown to have potential for the prediction of stroke outcome [5, 6]. The purpose of this study was to develop a prediction model with clinical factors and radiomics features and establish a nomogram as an individualized and evidence-based graphic guidance to predict the acute ischemic stroke (AIS) outcome.Methods
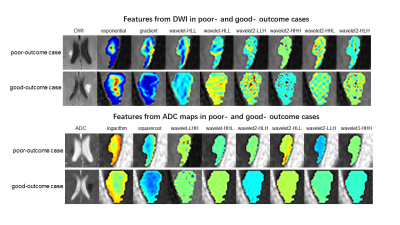
Data from 522 AIS patients between January 2013 to September 2019 were divided into the training (n=311) and validation cohort (n=211). The outcome of patients was determined by the 6-month modified Rankin Scale (mRS): good outcome (mRS≤2) and poor outcome (mRS>2). Radiomics features were extracted from diffusion-weighted image (DWI) and corresponding apparent diffusion coefficient (ADC) maps. The minimum redundancy maximum relevance algorithm and the least absolute shrinkage and selection operator logistic regression method were implemented to select features and establish radiomics score based on the constructed radiomics model. Univariate and multivariate logistic regression was performed to sift clinical factors and construct clinical model. Ultimately, a multivariate logistic analysis incorporating independent clinical factors and radiomics score was implemented to establish the final prediction model using backward stepdown selection procedure and a nomogram was developed. Its performance was evaluated by calibration, receiver operating characteristic (ROC) curves, precision-recall (PR) analysis and clinical utility.Results
Age, sex, stroke history, diabetes, mRSbaseline, baseline National Institutes of Health Stroke Scale score (NIHSSbaseline) and radiomics score were independent predictors of AIS outcome. The difference between the predictive efficacy of the radiomics model and the clinical model was not statistically significant. The prediction model yielded the greatest predictive performance with an AUC of 0.868 (95% CI 0.825-0.910) in the training cohort and 0.890 (95% CI 0.844-0.936) in the validation cohort, and the AUC-PR reached 0.733 and 0.787 respectively. The nomogram fitted well in the calibration curves (P > 0.05). Decision curve analysis demonstrated that the nomogram to predict AIS outcome provided a greater benefit than the clinical model when the threshold probability in clinical decision was greater than 0.06.Discussion
Age, NIHSSbaseline and mRSbaseline made up a larger proportion of the nomogram than other clinical features. Overall, the immunity of elderly patients was reduced; various complications were prone to occur; the NIHSSbaseline and mRSbaseline reflected the severity of stroke. In accordance with several studies, these factors are more stable and effective predictors [7, 8]. As diabetes leads to multi-organ pathologies and hyperglycemia and has negative effect on the fragile cerebral circulation during ischemia, it is strongly associated with death and recurrence after stroke[9]. Stroke history was also related with adverse events in stroke patients [10]. Consistent with the previous study [11], female is more likely to get poor outcome, attributed to an older age of onset in women, more severe stroke, a higher incidence of post-stroke depression, less social support and higher rates of immunosuppression after stroke[12]. The use of radiomics in the field of stroke prognosis is promising. Qiu et al.[13] demonstrated that patient recanalization could be better predicted compared to assessment of conventional thrombus imaging features such as length, volume, and permeability. Although Cui et al.[14] utilized radiomics features of six different magnetic resonance images and clinical factors to predict stroke outcome with AUC > 0.8, the time lag between onset and MRI scan was not clear in this study with only total sample size of 70 patients, far smaller than the sample size of our study. Tang et al.[15] constructed R score with radiomics features extracted from perfusion maps and DWI, and found that radiomics nomogram combining R score, clinical information and treatment options reached an AUC of 0.886 and 0.777 in predicting favorable outcome at 7 day and 3 months respectively after onset. Nevertheless, there was no significant difference between the AUC of the clinical nomogram and radiomics nomogram and the absence of the long-term clinical assessment in the training dataset lessened the evidence level. Wang et al.[16] developed a clinical-radiomics nomogram including age, NIHSS score at 24h post-admission, hemorrhage and radiomics score (only DWI used) to predict 3-month outcome of AIS patients with the final AUC of 0.80 and 0.73 respectively in the training and validation cohorts. The nomogram in our study incorporated more clinical factors such as sex, stroke history and diabetes, additionally we calculated corresponding ADC maps based on DWI and extracted more radiomics features and achieved an AUC of 0.868 and 0.890 in the training and validation cohorts as more splendid prediction performance.Conclusions
The nomogram incorporated with clinical factors and radiomics features achieved satisfactory prediction for AIS outcome. It could assist clinicians to formulate individual treatment plans at the early stage of onset, which may significantly improve the ultimate outcome of the AIS patients.Acknowledgements
This work was supported by the National Natural Science Foundation of China (grant No:81730049).References
References:
1. Campbell B, Khatri P (2020) Stroke. Lancet 396:129-142
2. Barber PA, Powers W (2006) MR DWI does not substitute for stroke severity scores in predicting stroke outcome. Neurology 66:1138-1139
3. Kocak B, Durmaz ES, Ates E, et al. (2020) Radiogenomics of lower-grade gliomas: machine learning–based MRI texture analysis for predicting 1p/19q codeletion status. Eur Radiol 30:877-886
4. Park CJ, Han K, Kim H, et al. (2020) Radiomics risk score may be a potential imaging biomarker for predicting survival in isocitrate dehydrogenase wild-type lower-grade gliomas. Eur Radiol 30:6464-6474
5. Kassner A, Liu F, Thornhill RE, et al. (2009) Prediction of hemorrhagic transformation in acute ischemic stroke using texture analysis of postcontrast T1-weighted MR images. J Magn Reson Imaging 30:933-941
6. Betrouni N, Yasmina M, Bombois S, et al. (2020) Texture Features of Magnetic Resonance Images: an Early Marker of Post-stroke Cognitive Impairment. Transl Stroke Res 11:643-652
7. Ali SF, Siddiqui K, Ay H, et al. (2016) Baseline Predictors of Poor Outcome in Patients Too Good to Treat With Intravenous Thrombolysis. Stroke 47:2986-2992
8. Rost NS, Bottle A, Lee JM, et al. (2016) Stroke Severity Is a Crucial Predictor of Outcome: An International Prospective Validation Study. J Am Heart Assoc 5
9. Echouffo-Tcheugui JB, Xu H, Matsouaka RA, et al. (2018) Diabetes and long-term outcomes of ischaemic stroke: findings from Get With The Guidelines-Stroke. Eur Heart J 39:2376-2386
10. Andrew N, Kilkenny M, Harris D, et al. (2014) Outcomes for People with Atrial Fibrillation in an Australian National Audit of Stroke Care. Int J Stroke 9:270-277
11. Lisabeth LD, Reeves MJ, Baek J, et al. (2015) Factors Influencing Sex Differences in Poststroke Functional Outcome. Stroke 46:860-863
12. Reeves MJ, Bushnell CD, Howard G, et al. (2008) Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol 7:915-926
13. Qiu W, Kuang H, Nair J, et al. (2019) Radiomics-Based Intracranial Thrombus Features on CT and CTA Predict Recanalization with Intravenous Alteplase in Patients with Acute Ischemic Stroke. Am J Neuroradiol 40:39-44
14. Cui H, Wang X, Bian Y, et al. (2018) Ischemic stroke clinical outcome prediction based on image signature selection from multimodality data. Conference proceedings (IEEE Engineering in Medicine and Biology Society. Conf.) 2018:722
15. Tang T, Jiao Y, Cui Y, et al. (2020) Penumbra-based radiomics signature as prognostic biomarkers for thrombolysis of acute ischemic stroke patients: a multicenter cohort study. J Neurol 267:1454-1463
16. Wang H, Sun Y, Ge Y, et al. (2021) A Clinical-Radiomics Nomogram for Functional Outcome Predictions in Ischemic Stroke. NEUROLOGY AND THERAPY
Figures