4587
The impact of hemodynamic patterns and geometric features of vertebra-basilar system on atherosclerotic plaque occurrence1Center for Biomedical Imaging Research, Tsinghua University, Beijing, China, 2Fujian Medical University Union Hospital, Fuzhou, Fujian Province, China, 3Department of Biomedical Engineering, School of Life and Science, Beijing Institute of Technology, Beijing, China, 4Department of Radiology, Fujian Medical University Union Hospital, Fuzhou, Fujian, China
Synopsis
This study investigated the relationship between the geometry of vertebra-basilar system and hemodynamic measurements and presence of BA plaques. We found that geometric measurements and most hemodynamic features were significantly correlated with the occurrence of BA plaque (mean curvature, r=0.368; NOR-TAWSS-NF, r=-0.312; SAR-OSI-NF, r=0.290; NOR-TAWSS-nNF, r=-0.387; NOR-OSI-nNF, r=0.440). There were significant differences in mean curvature, hemodynamic characteristics of Newtonian flow and non-Newtonian flow models between patients with and without BA plaque. Our study indicated that geometric features and non-Newtonian flow model-based hemodynamic measurements are risk factors of BA plaque.
Introduction
Approximately 80% of strokes are attributed to the ischemic origin, of which 20% to 25% are located in the posterior circulation1. The posterior circulation is generally supplied by the vertebra-basilar system. The most common sites of atherosclerotic diseases are the basilar artery (BA), vertebral artery (VA) and posterior cerebral artery (PCA) in the vertebra-basilar system2. Geometric characteristic and hemodynamic features have been generally considered as strong indicators for carotid atherosclerosis3, 4. Considering characteristics of nature of tortuosity and smaller vessel size of intracranial arteries and complex patterns of blood flow, non-Newtonian flow model might be more appropriate for analyzing the patterns of intracranial hemodynamics. This study aimed to investigate the association of geometry and hemodynamics of vertebra-basilar system with the presence of BA plaque by using MR imaging, geometric analysis and computed fluid dynamic (CFD) simulation.Methods
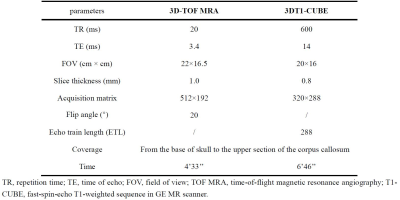
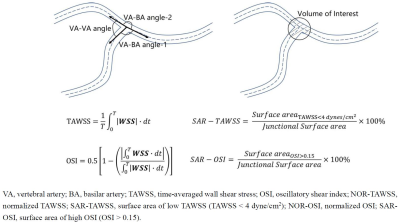
Study sample: Patients with a recent posterior circulation ischemic stroke (within 2 weeks) were recruited in this study. The study protocol was approved by institutional review board and written consent form was obtained from all patients. MR imaging protocol and image analysis: All the patients underwent MR vessel wall imaging for intracranial arteries on a 3.0T MR scanner (Discovery MR750, General Electric Medical System, Milwaukee, WI, USA) with 8-channel head coil. The detailed imaging parameters are listed in Table 1. The MR vessel wall images of the vertebra-basilar artery were interpreted by 2 experienced radiologists (> 5 years’ experience in vascular imaging) using Explorer software (TSImaging, Beijing, China). The contours of arterial lumen were traced and presence of basilar arterial plaque was identified which is defined as eccentric wall thickening lesion. Geometric model and analysis: The 3D geometric structure vertebro-basilar system was reconstructed through a commercial vascular modeling toolkit (VMTK 1.4.0, OROBIX SRL). Demonstrated in Figure 1, the geometrical features including mean and max curvature of vertebral arteries and bifurcation angle were measured and the hemodynamics were extracted in the vertebra-basilar junction. CFD model and analysis: Based on the 3D geometric models, the reconstructed model was meshed into 1~2 million elements by ICEM CFD (ANSYS 19.2 Inc., USA) with prismatic cells in the 5 boundary layers near the vessel wall. In the CFD simulation, both Newtonian flow (NF) and non-Newtonian flow (nNF) were applied to extract hemodynamic features of the vertebra-basilar junction. The velocity of vessel inlet and pressure of vessel outlets were extracted from numerous volunteers’ data. CFX (ANSYS 19.2 Inc., USA) was used to solve the Navier-Stokes model. To evaluate the mechanical influence of the flow, surface area ratio of low time-averaged WSS (SAR-TAWSS), surface area ratio of high oscillatory shear index (SAR-OSI), surface normalized time-averaged WSS (NOR-TAWSS) and surface normalized OSI (NOR-OSI) were applied to this study. Statistical analysis: Spearman correlation analysis was conducted to calculate the correlation coefficients between the geometry and hemodynamic features of vertebra-basilar system and presence of BA plaque. Independent t test or Mann-Whitney U test was used to compare the geometry and hemodynamics of vertebra-basilar system between patients with and without BA plaque. All statistical analyses were conducted using SPSS 26.0 (SPSS Inc. Chicago, IL, USA).Results
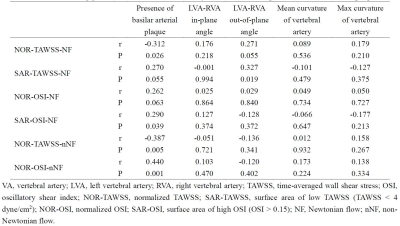
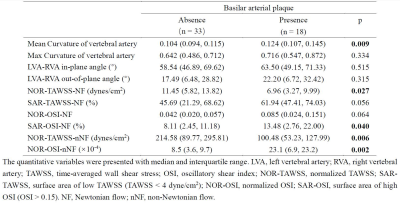
In this study, a total of 51 patients (mean age: 70.4±8.7 years, 34 males) were enrolled. The correlation coefficients between geometry, hemodynamic characteristics and occurrence of BA plaque are illustrated in Table 2. Most hemodynamic features were significantly correlated with the occurrence of BA plaque (NOR-TAWSS-NF, r=-0.312, p=0.026; SAR-OSI-NF, r=0.290, p=0.039; NOR-TAWSS-nNF, r=-0.387, p=0.005; NOR-OSI-nNF, r=0.440, p=0.001). Meanwhile, the correlation coefficient between VA junction bifurcation angle and SAR-TAWSS-NF was 0.327 (p=0.019) and mean curvature of VA was significantly associated with presence of BA plaque (r = 0.368, p = 0.008). Table 3 presented the results on comparing hemodynamic measurements and geometry between patients with and without BA plaque. Compared to patients without BA plaque, those with BA plaque had significantly greater mean curvature (median: 0.124 vs. 0.104, p=0.009), SAR-OSI-NF (median: 13.48% vs. 8.11%, p=0.040), NOR-OSI-nNF (median: 23.1×10-4 vs. 8.5×10-4, p=0.002) and lower NOR-TAWSS-NF (median: 6.96 dynes/cm2 vs. 11.45 dynes/cm2, p=0.027) and NOR-TAWSS-nNF (median: 100.48 dynes/cm2 vs. 214.58 dynes/cm2, p=0.006).Discussion and Conclusion
In this study, both geometrical features and hemodynamics of vertebra-basilar system were found to be associated with presence of BA plaque. Hemodynamic measurements from non-Newtonian flow model are more closely associated with the occurrence of BA plaque than those from Newtonian flow model. Our findings suggested that TAWSS and OSI of vertebra-basilar system might he potential indicators for presence of BA plaques. In a patient-specific study, Yin et al found that hemodynamic measurements of local area near the vertebral junction are associated with the atherosclerotic plaques5. However, such study only enrolled 6 patients. In contrast, the present study enrolled 51 patients and only NOR-TAWSS and SAR-OSI were found to be significantly associated with presence of BA plaques. From the aspect of fluid dynamics, geometrical changes would lead to variation of local hemodynamic patterns. When such difference occurred in the junction or bifurcation, the environment with low TAWSS and high OSI would promote the formation of plaques, especially in intracranial arteries with non-Newtonian blood flow. Out findings also suggested that non-Newtonian flow model would be better for CFD analysis of intracranial arteries.Acknowledgements
No acknowledgement found.References
1. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease. Stroke, 2011, 42(8):E464-540.
2. Qureshi AI, Caplan LR. Intracranial atherosclerosis. Lancet. 2014;383(9921):984-998.
3. Zheng J, Sun B, Lin R, Teng Y, Zhao X, Xue Y. Association between the vertebrobasilar artery geometry and basilar artery plaques determined by high-resolution magnetic resonance imaging. BMC Neurosci. 2021;22(1):20.
4. Zhou L, Yan Y, Du H, Ni X, Wang G, Wang Q. Plaque features and vascular geometry in basilar artery atherosclerosis. Medicine (Baltimore). 2020;99(18):e19742.
5. Yin X, Huang X, Feng Y, Tan W, Liu H, Huo Y. Interplay of Proximal Flow Confluence and Distal Flow Divergence in Patient-Specific Vertebrobasilar System. PLoS One. 2016;11(7):e0159836.
Figures