4586
Improve the Image Quality of Arterial Spin Labeling with Echo Planar Imaging with Compressed SENSE1Department of Radiology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2Philips Healthcare, Shanghai, China
Synopsis
Arterial spin labeling (ASL) is a non-invasive MRI perfusion technique that can quantify tissue blood flow, which is meaningful for clinical applications. However, ASL perfusion images always have a limited signal-to-noise ratio (SNR). We aimed to using the echo planar imaging with compressed SENSE (EPICS) to obtain high-quality brain ASL images. Eleven healthy subjects and four patients with intracranial infarction were enrolled, and underwent ASL imaging with and without EPICS. The results demonstrated the feasibility of EPICS to increase the quality of ASL images.
Introduction
Arterial spin labeling (ASL) is a non-invasive MRI perfusion technique that can quantify tissue blood flow1-2. Compare with 3D pseudo continuous arterial spin labeling (pCASL), clinical 2D pCASL images based on echo planar imaging (EPI) are insensitive to image artifacts from motion but with limited signal-to-noise ratio (SNR)3. Compressed SENSE (CS) was initially introduced to MRI to increase scanning speed, for its ability to reconstruct images accurately from highly under-sampled data4. The CS reconstruction can also combine with EPI, to improve image quality for high-resolution DWI5. In this study, we attempted to using the echo planar imaging with compressed SENSE (EPICS) to obtain high-quality brain ASL and to demonstrate the feasibility of EPICS-ASL.Method
Eleven healthy subjects (3 males, 8 females; mean age, 39.55 years ± 11.62 [standard deviation]; range, 23 to 57 years) without known cerebrovascular disease and four patients (4 males; mean age, 60.25 years ± 9.91 range, 48 to 70 years) with intracranial infarction were scanned as part of this study. 2D pCASL was acquired in subjects with an axial single-shot, spin-echo, echo-planar imaging sequence, on a 3.0T MRI system (Ingenia CX, Philips Healthcare, Best, the Netherlands). The sequence used the following parameters: repetition time (TR) = 4550 ms, echo time (TE) = 12 ms, pixel size = 2.7 × 2.7 mm2, slice thickness = 5.0 mm, FOV = 240 × 240 × 95 mm3, SENSE factor or CS-SENSE factor = 2.3. ASL imaging with and without EPICS were sampled with same scanning time. Signal-to-noise ratio (SNR) was determined by the ratio between the mean signal intensity inside the ROI (SROI) and the standard deviation of the background noise (σBG) (SNR = SROI/σBG). We performed the SNR of basal ganglia, white matter, grey matter, brain stem, cerebellum and Infarction for patients. Then, all images were rated according to a scale that ranged from 1 (unacceptable image quality) to 4 (artifact-free image without distortions and with high-level anatomic detail). Similarly, for the patients, infarction boundary was rated according to a scale that ranged from 1 to 3 (1: cannot be displayed; 2: the boundary is blurred; 3: the boundary is clear). Differences in SNR between EPICS-ASL and EPI-ASL images were assessed using two-sided t tests, and image quality and infarction boundary were assessed using Wilcoxon signed rank test.Result
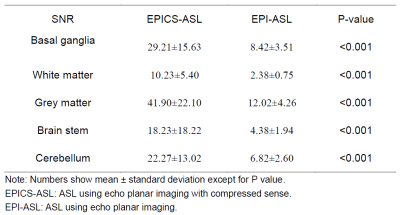
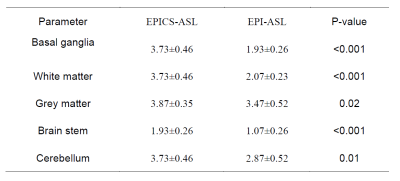
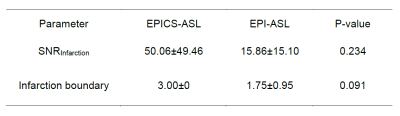
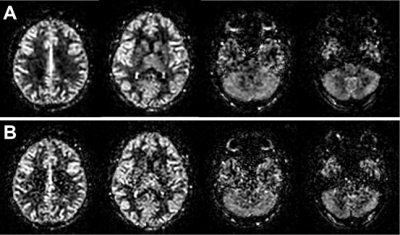
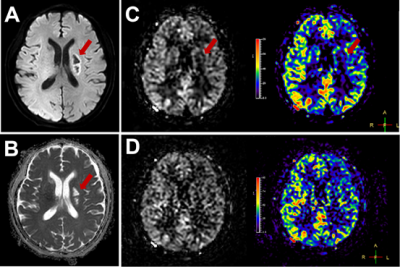
The EPICS-ASL was superior to EPI-ASL regarding the SNR (P<0.05), and image quality in the basal ganglia, white matter, grey matter, brain stem, and cerebellum (P<0.05). Detailed qualitative comparison of SNR and image quality between EPICS-ASL and EPI-ASL is shown in Table 1 and Table 2. Representative EPICS-ASL and EPI-ASL images of a healthy subjects are shown in Figure 1. The EPICS-ASL image demonstrated increased SNR of infraction and infarction boundary compared with EPI-ASL images in patients. Detailed qualitative comparison is shown in Table 3. Representative EPICS-ASL and EPI-ASL images of a patient with chronic ischemic stroke in left basal ganglia was shown in Figure 2.Discussion
ASL is a non-invasive MRI perfusion technique meaningful for clinical applications. However, 2D pCASL images based on EPI always have a limited SNR. In this study, we obtained high-quality 2D brain ASL images by combining the EPI with CS reconstruction. The results demonstrated the feasibility of EPICS to increase the quality of ASL images. However, there are still some limitations in our research. For example, we didn’t compare 2D EPICS-ASL with 3D pCASL, which is more commonly used in clinical application for its higher SNR and better background suppression efficiency.Conclusion
The EPICS-ASL was superior to EPI-ASL in the SNR and image quality. EPICS-ASL could improve the image quality of brain ASL and may help to accurately evaluate the cerebral perfusion.Acknowledgements
No acknowledgement found.References
1. Göttler J, Kaczmarz S, Kallmayer M, et al. Flow-metabolism uncoupling in patients with asymptomatic unilateral carotid artery stenosis assessed by multi-modal magnetic resonance imaging[J]. Journal of Cerebral Blood Flow & Metabolism, 2019, 39(11): 2132-2143.
2. Detre J A, Rao H, Wang D J J, et al. Applications of arterial spin labeled MRI in the brain[J]. Journal of Magnetic Resonance Imaging, 2012, 35(5): 1026-1037.
3. Alsop D C, Detre J A, Golay X, et al. Recommended implementation of arterial spin‐labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia[J]. Magnetic resonance in medicine, 2015, 73(1): 102-116.
4. Lustig M, Donoho D, Pauly J M. Sparse MRI: The application of compressed sensing for rapid MR imaging[J]. Magnetic Resonance in Medicine: An Official Journal of the International Society for Magnetic Resonance in Medicine, 2007, 58(6): 1182-1195
5. Kaga T, Noda Y, Mori T, et al. Diffusion-weighted imaging of the abdomen using echo planar imaging with compressed SENSE: Feasibility, image quality, and ADC value evaluation[J]. European Journal of Radiology, 2021, 142: 109889.
Figures