4583
Are cerebral microvascular perfusion and diffusion dynamics associated with neurological function in acute ischemic stroke?1Department of Radiology, the Yancheng School of Clinical Medicine of Nanjing Medical University, Yancheng, China, 2Department of Neurology, the Yancheng School of Clinical Medicine of Nanjing Medical University, Yancheng, China, 3GE Healthcare, MR Research China, Beijing, China
Synopsis
This work explored the association of cerebral microvascular perfusion and diffusion dynamics measured by intravoxel incoherent motion (IVIM) imaging with initial neurological function and clinical outcome in acute stroke patients. Significant negative correlations were revealed between IVIM derived diffusion dynamics parameters and initial neurological function as well as clinical outcome for patients with acute ischemic stroke. However, no similar statistical correlation was found for parameters related to microvascular perfusion. IVIM may be therefore suggested as an effective non-invasive method for evaluating the initial neurological function and clinical outcome in acute ischemic stroke.
Introduction
Stroke has become the leading cause of death in China as well as the second leading cause of death in the world.1 Neuroimaging is an important tool in clinical diagnosis and treatment evaluation of acute ischemic stroke. Among various neuroimaging techniques,magnetic resonance diffusion weighted imaging (DWI) has been widely applied for detecting acute stroke in clinic.2 Restricted diffusion of ischemic lesion has been found to attribute to the restricted motion of molecular diffusion of water and microvascular perfusion in the capillary network, separately.3Intravoxel incoherent motion (IVIM) DWI, as an attractive multi-b values diffusion imaging technique, is able to separate tissue diffusivity and perfusion-related diffusivity.3,4 So far, the relationship between both microvascular perfusion and diffusion dynamics measured by IVIM and initial neurological function as well as clinical outcome remains uncertain for acute ischemic stroke patients.
Therefore, the main purpose of this work was to evaluate the relationships of the corresponding IVIM parameters with initial neurological function and clinical outcome.
Materials and Methods
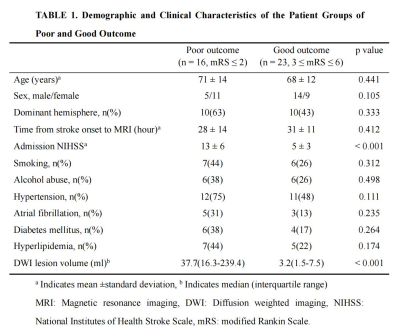
In total, 39 patients (Female/Male 20/19, Age 69 ± 13 years old) were recruited in this study and assessed with admission National Institutes of Health Stroke Scale (NIHSS) and day-90 modified Rankin Scale (mRS). According to mRS scoring, poor outcome group (3 ≤ day-90 mRS ≤ 6) and good outcome group (day-90 mRS ≤ 2) were defined.All MR experiments were performed on an 3T MR scanner (HDxt, GE), with an eight channel coil employed. The imaging parameters of IVIM were set as follows: TR = 5825 ms, TE = 94 ms, FOV = 24 × 24 cm2, slice thickness/gap = 5 mm/1.5 mm, matrix size = 128 × 128, acceleration factor = 2, b values = 0, 10, 20, 40, 80, 110, 140, 170, 200, 300, 400, 500, 600, 800, 1000 s/mm2, and acquisition time = 7 min 11 s.
Post-processing of IVIM data were implemented through a vendor-provided workstation (AW 4.5, GE Healthcare). The corresponding parametrical maps were obtained, including apparent diffusion coefficient (ADC), pseudo-diffusion coefficient (D*), true diffusion coefficient (D) and perfusion fraction (f). The fD* was the product of f and D*. Two neuroradiologists, blinded to clinical data, were employed for data evaluation. Regions of interest (ROI)s were manually drawn in the ischemic core (hyperintensities on each slice of diffusion images (b-value = 1000 s/mm2)), and then copied to each IVIM parametrical maps. The ratios of lesioned/contralateral parameters (rADC, rD, rD*, rf and rfD*) were also obtained.
All statistic analyses were performed on SPSS software. The intraclass correlation coefficient (ICC) was used to evaluate the inter-observer agreement of IVIM parameter and lesion volume over two radiologists. An independent t-test was used to test the differences of each parameter between the good and poor outcome groups. Partial correlation analysis was used to evaluate the correlations between the admission NIHSS / day-90 mRS and each parameter ratio, with lesion volumes controlled. P<0.05 was considered statistic significant threshold.
Results
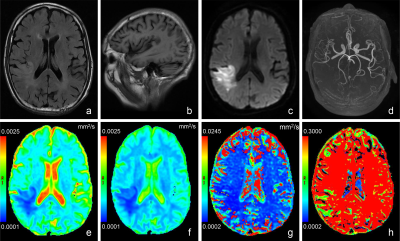
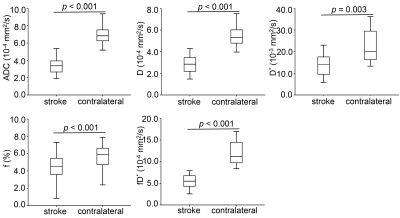
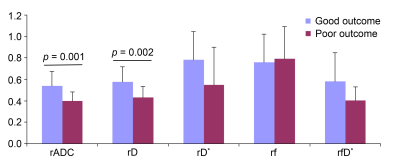
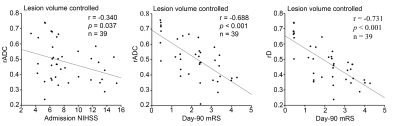
Conventional anatomic MRI and multiple parametric maps of IVIM were shown for a representative patient with acute ischemic stroke (Fig. 1). Table 1 summarizes the demographic and clinical characteristics of patients. The ICC values of D*, f, D, ADC and lesion volumes were 0.770, 0.773, 0.880, 0.891 and 0.995, respectively. The ADC, D, D*, f and fD* values of lesions were significantly reduced than those of the contralateral regions (all p < 0.01;Fig. 2). The rADC and rD were significantly decreased in poor than good outcome group (all p < 0.01;Fig. 3). With lesion volume controlled, rADC showed a weak negative correlation (r = -0.340, p = 0.037) and a notable negative correlation (r = -0.688, p < 0.001) with admission NIHSS score and day-90 mRS score, respectively (Fig. 4). In addition, rD showed a strong negative correlation (r = -0.731, p < 0.001) with day-90 mRS score (Fig. 4).Discussion and conclusion
This study was a first attempt to simultaneously explore the associations of cerebral microvascular perfusion and diffusion dynamics with neurological function on admission and clinical outcome of acute ischemic stroke. Both diffusion-related parameters and microvascular perfusion-related parameters showed significantly decreased values in ischemic lesions than at contralateral regions. These findings in acute ischemic stroke assessment were similar to those reported previously. 3,5 However, conflicted D* dynamics in ischemic lesions were reported in previous studies. This discrepancy might be explained by the following aspects: Firstly, inter-subject difference, such as the partial volume effect of cerebrospinal fluid, might limit the robustness of IVIM derived perfusion parameter of D*.3 Secondly, not standardized scan protocol of IVIM imaging.3,5 While lesion volume as a confounding factor was controlled, rADC showed a notable negative correlation with day-90 mRS score. Furthermore, we also found a strong negative correlation between rD and day-90 mRS score with lesion volume controlled. Interestingly, this negative correlation was not found between rD and initial neurological function. It is likely that rADC includes more complicated information and better represents the early pathophysiological changes after acute ischemic stroke, however, rD has a stronger negative correlation with clinical outcome.In conclusion, IVIM may be suggested as an effective non-invasive method for evaluating the initial neurological function and clinical outcome in acute ischemic stroke.
Acknowledgements
This work was supported by the Programs of Scientific Research Project of Jiangsu Commission of Health of China (No. H2019088), the Foundation Plan for Outstanding People of The Sixth Peak of Jiangsu Province of China (No. 2019-WSN-313), the Foundation Plan for The Fifth Scientific Research Project of “333 Project” of Jiangsu Province of China (No. BRA2019031) and GE Healthcare.References
1. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145-1158.
2. Heiss WD, Zaro-Weber O. Extension of therapeutic window in ischemic stroke by selective mismatch imaging. Int J Stroke. 2019;14(4):351-358.
3. Zhu G, Federau C, Wintermark M, et al. Comparison of MRI IVIM and MR perfusion imaging in acute ischemic stroke due to large vessel occlusion. Int J Stroke. 2020;15(3):332-342.
4. Liu C, Zhang S, Yao Y, et al. Associations Between Diffusion Dynamics and Functional Outcome in Acute and Early Subacute Ischemic Stroke. Clin Neuroradiol. 2020;30(3):517-524.
5. Yao Y, Zhang S, Tang X, et al. Intravoxel incoherent motion diffusion-weighted imaging in stroke patients: initial clinical experience. Clin Radiol. 2016;71(9):938.e11-6.
Figures