4579
ATP-A safe stressor for stress perfusion cardiac magnetic resonance1Radiology, Beijing Friendship Hospital, Beijing, China, 2Siemens Healthcare, Beijing, China, 3Beijing Friendship Hospital, Beijing, China, 4Beijing Anzhen Hospital, Beijing, China
Synopsis
This study investigated the side effects and safety of ATP as a stressor for stress perfusion cardiac magnetic resonance. The result showed the high safety of stress perfusion with ATP and side effects were mild and resolved shortly after receiving ATP. Furthermore, it was also observed splenic switch-off that can be used to assess stress adequacy undergoing stress-CMR with ATP.
Purpose • Method • Result • Conclusion • References • Acknowledgements
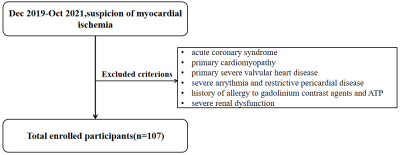
Purpose:Stress perfusion cardiac magnetic resonance(S-CMR) is a non-invasive imaging modality to detect coronary stenosis and assess impaired blood flow reserve in coronary artery disease(CAD), with high sensitivity, specificity and accuracy[1, 2].The currently more applied stressors are adenosine and regadenoson. Another stressor adenosine triphosphate (ATP), a phosphorylation product of adenosine, has vasodilolic and hemodynamic changes similar to adenosine. Although ATP is a readily accessible and cheap relative to other stressors, it is less used worldwide. Our study used ATP as a stressor, evaluating its stress effect and safety, which has not been previously reported. It provides an option for subsequent S-CMR[2].Methods:We performed a retrospective study from December 2019 and October 2021 and included 107 subjects with suspected non-obstructive coronary artery disease (NOCAD). Those patients always had symptoms of myocardial ischemia and inclusion and exclusion criteria are as Figure 1.[3-6].They were underwent ATP stress perfusion CMR on a 3T MR scanner( MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) which including cine, ATP stress and rest perfusion, and late gadolinium enhancement (LGE) imaging[7]. Patients were given ATP at an infusion rate of 0.16 mg/kg/min for approximately 2 minutes (heart rate increase≥10 bpm or systolic blood pressure decrease≥10 mmHg) achieving an appropriate hemodynamic response.Then the injection was continued for 2 minutes to obtain stress perfusion images using a T1 weighted fast gradient echo sequence (TR/TE = 2.1/1.03ms, TI = 100 ms, temporal resolution = 155.7ms, flip angle = 10°; voxel size=1.9×1.9×8.0mm3). Cine images were acquired by a balanced steady state free-precession(bSSFP) sequence (TR/TE = 3.3/1.43ms, temporal resolution = 40ms, flip angle = 50°; voxel size=1.6×1.6×6.0mm3). Rest perfusion images were acquired at least 10 min after termination of ATP infusion. The LGE parameters were: TR/TE = 5.2/1.96ms, TI = 300 ms, flip angle = 20°;voxel size=1.8×1.8×8.0mm3.We investigated side effects and splenic switch‑off (SSO) in patients using ATP as a stressor[8-10]. Qualitative myocardial perfusion analysis was that an inducible ischemia was defined as the presence of a stress perfusion defect, in absence of matching LGE, in≥1segment that persisted for≥6 beats.And semin-quantitative myocardial perfusion images were analyzed by dedicated CMR software cvi42 (Circle Cardiovascular Imaging, Calgary, Canada).
Results:A total of 107 patients were enrolled (53±11 years of age, 38% women), 3 patients stopped scanning due to atrioventricular block. Most patients had one or more cardiovascular risk factor, such as hypertension, smoking history, or hypercholesterolemia as shown in Table 1.Out of 104 patients,7 patients’ images were excluded(3 patients were not injected gadolinium during scanning, 3 patients’ images was not first-pass perfusion,1patient’ image quality was poor).After a qualitative and semi-quantitative comprehensive analysis, 79 patients had reversible myocardial ischemia,a typical example as figure 2. During pharmacologically induced stress, 31 patients (29%) experienced symptoms during ATP infusion. Side-effects included chest pain, flushing, dyspnea, headache and atrioventricular block as Table 2. Symptoms were mild and resolved shortly after receiving ATP. No myocardial infarction and bronchospasm were observed. And adequate splenic tissue for analysis was seen in 96% of the myocardial perfusion examinations (4 patients were excluded due to not scan the spleen). Splenic switch-off with ATP was present in 91% (91/100) of the ATP perfusion MR studies. One representative case was shown in Figure 3.
Conclusion:ATP is a potent coronary vasodilator that can be safely used for stress perfusion CMR. ATP has a short time to take effect(about 2minutes)and causes mild side effects. Splenic switch-off can be used to assess stress adequacy in patients undergoing stress-CMR with ATP.
Acknowledgements
We sincerely thank the participants in this study.References
[1] Eike N M D, John P G M D, Gerry P M M D, et al. Magnetic Resonance Perfusion or Fractional Flow Reserve in Coronary Disease[J]. New England Journal of Medicine,2019,380(25).
[2] Zamorano J L, Pinto F J, Solano-López J, et al. The year in cardiovascular medicine 2020: imaging[J]. European Heart Journal,2021,42(7):740-749.
[3] Ong P, Seitz A. Advances in Risk Stratification of Patients With Coronary Microvascular Dysfunction[J]. JACC: Cardiovascular Imaging,2021,14(3):612-614.
[4] Mathew R C, Bourque J M, Salerno M, et al. Cardiovascular Imaging Techniques to Assess Microvascular Dysfunction[J]. JACC: Cardiovascular Imaging,2020,13(7):1577-1590.
[5] Kwong R Y, Ge Y, Steel K, et al. Cardiac Magnetic Resonance Stress Perfusion Imaging for Evaluation of Patients With Chest Pain[J]. Journal of the American College of Cardiology,2019,74(14):1741-1755.
[6] Marcos-Garces V, Gavara J, Monmeneu J V, et al. Vasodilator Stress CMR and All-Cause Mortality in Stable Ischemic Heart Disease[J]. JACC: Cardiovascular Imaging,2020,13(8):1674-1686.
[7] Tian J, Zhang L, Yang X, et al. The effect of Shexiang Tongxin Dropping Pills on coronary microvascular dysfunction (CMVD) among those with a mental disorder and non-obstructive coronary artery disease based on stress cardiac magnetic resonance images: A study protocol[J]. Medicine (Baltimore),2020,99(21):e20099.
[8] Garcia-Baizan A, Millor M, Bartolome P, et al. Adenosine triphosphate (ATP) and adenosine cause similar vasodilator effect in patients undergoing stress perfusion cardiac magnetic resonance imaging[J]. Int J Cardiovasc Imaging,2019,35(4):675-682.
[9] Hosking A, Koulouroudias M, Zemrak F, et al. Evaluation of splenic switch off in a tertiary imaging centre: validation and assessment of utility[J]. Eur Heart J Cardiovasc Imaging,2017,18(11):1216-1221.[10] Manisty C, Ripley D P, Herrey A S, et al. Splenic Switch-off: A Tool to Assess Stress Adequacy in Adenosine Perfusion Cardiac MR Imaging[J]. Radiology,2015,276(3):732-740.
Figures