4575
Multi-delay arterial spin labeling perfusion map may predict cerebral hyperperfusion after carotid endarterectomy1Peking Union Medical College Hospital, Beijing, China, 2GE healthcare, Beijing, China
Synopsis
Preoperative measurement of cerebrovascular reactivity using acetazolamide or CO2 induced SPECT is the gold standard for predicting cerebral hyperperfusion (CH) after carotid endarterectomy (CEA). However, it is often impractical to perform SPECT examinations on all patients.
Arterial spin labeling (ASL) is a non-invasive technique to image the brain perfusion. Based on multi-delay ASL perfusion map, we extracted two hemodynamic parameters (cerebral blood flow and arterial transit time) and established a five-scale scoring system for the prediction of CH.
We found in patients with carotid stenosis, multi-delay ASL is a practical and reliable tool for the prediction of CH after CEA.
Objectives
Arterial spin labeling (ASL) is a non-invasive technique to image the brain perfusion [1], which is sensitive to stenosis and collateral circulation [2-3]. we aimed to investigate whether hemodynamic information derived from multi-delay ASL MRI can predict cerebral hyperperfusion (CH) after carotid endarterectomy (CEA).Methods
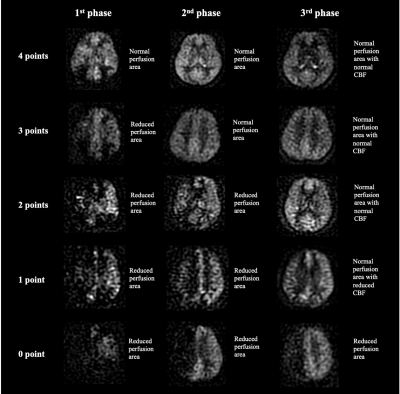
Consecutive patients with carotid stenosis who underwent CEA between August 2020 and October 2021 were included. CH was defined as an increase in cerebral blood flow (CBF) > 100% compared with preoperative values [4]. Patients were divided into CH and non-CH groups. Multi-delay arterial spin labeling MRI was performed within 30 days before CEA. With three post-labeling delays (1.0, 1.57, 2.46s), preoperative ASL images generated three phases of perfusion maps. Two neuroradiologists independently graded ASL images by using a five-scale scoring system (Figure 1). This multi-delay ASL score was correlated with arterial transit time (ATT) and CBF in ipsilateral middle cerebral artery territory. The relationship between CH and ASL parameters (ATT, CBF and multi-delay ASL score) were also examined by t test, Mann-Whitney U test and ROC curve analysis.Results
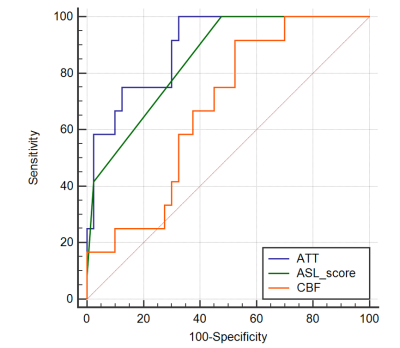
A total of 52 patients were included (mean age 65±7.6 years, 80.8% male). CH was observed in 12 (23.1%) patients. Multi-delay ASL score was negatively correlated with ATT (r = -0.63, p<0.001) and positively correlated with CBF (r = 0.40, p=0.004). Patients in CH-group had significantly longer ATT (1668.0±67.0ms vs 1493.2±129.7ms, p<0.001), lower CBF (27.8±6.2mL/100g/min vs 33.0±7.6mL/100g/min, p=0.036) and lower multi-delay ASL score (2 [1,2] vs 3 [2,3.75], p<0.001). None of patients with 3 or 4 points ASL score developed CH after CEA. The multi-delay ASL score (AUC=0.85 [0.724,0.934]) performed better than CBF (AUC=0.675 [0.531,0.798], p=0.025) and as well as ATT (AUC=0.896 [0.78,0.963], p=0.423) for the prediction of CH (Figure 2).Conclusion
In patients with carotid stenosis, multi-delay ASL is a practical and reliable tool for the prediction of CH after CEA.Acknowledgements
We thank Juan Wei from GE Healthcare, Beijing, China for MRI technique help.References
1.Alsop DC, Detre JA, Golay X, Günther M, Hendrikse J, Hernandez-Garcia L et al (2015) Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med 73:102–116.
2.Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME, Steinberg GK (2011) Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with moyamoya disease. Stroke 42:2485-2491.
3.Monitoring cerebral perfusion changes after revascularization in patients with Moyamoya disease by using arterial spin-labeling MR Imaging. Radiology 288:565-572.
4. van Mook WN, Rennenberg RJ, Schurink GW, van Oostenbrugge RJ, Mess WH, Hofman PA et al (2005) Cerebral hyperperfusion syndrome. Lancet Neurol 4:877-888.