4574
Collateral Circulation Detected by Arterial Spin Labeling Can Predict Outcome in Acute Ischemic Stroke1Department of Neurology, Affiliated ZhongDa Hospital, School of Medicine, Southeast University, Nanjing, Jiangsu, China
Synopsis
Robust collateral circulation is strongly associated with better outcomes in acute ischemic stroke. In this prospective study, collateral circulation was defined as arterial transit artifact in Arterial Spin Labeling(ASL) images. Patients with ASL collaterals represented higher rate of good outcome and there were significant differences for percent changes of mRS score and NIHSS score between groups. Furthermore, the presence of ASL collaterals could predict good outcome, even after controlling for baseline NIHSS score. Taken together, ASL collaterals provide a powerful tool to predict clinical outcome for acute ischemic stroke with 90 days follow-up.
Abstract
INTRODUCTION Stroke is a major cause of mortality and disability globally1. Most strokes are ischemic, of which restoring blood flow of ischemic penumbra is a key point of therapy. Robust collateral circulation is strongly associated with better outcomes in acute ischemic stroke (AIS)2-4. The generally accepted gold standard for assessing collateral circulation is digital subtraction angiography (DSA), which is limited by the defects including invasiveness and expensiveness. Hence, noninvasive techniques are definitely needed to assess collateral circulation. The goal of this study was to determine whether collateral circulation detected by arterial spin labeling (ASL) magnetic resonance imaging predicts better clinical outcome in AIS patients with 90 days follow-up.METHODS In this prospective study, AIS patients were obtained from October 2018 to February 2021. Collateral circulation was defined as arterial transit artifact(ATA)5 in ASL images. Modified rankin scale (mRS), the Barthel Index (BI), and national institutes of health stroke scale (NIHSS) were employed to evaluate neurological function, the percent change of which was calculated respectively. In this study, the clinical outcome were perceived to be favorable when follow-up mRS score was 0-2. Receiver operating characteristic curve (ROC curve) was performed to estimate the predictive value.
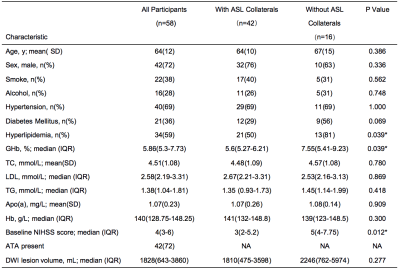
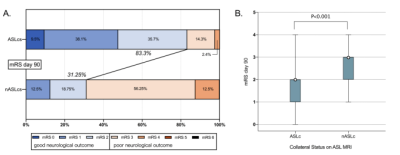
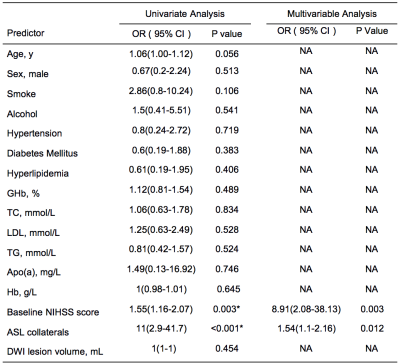
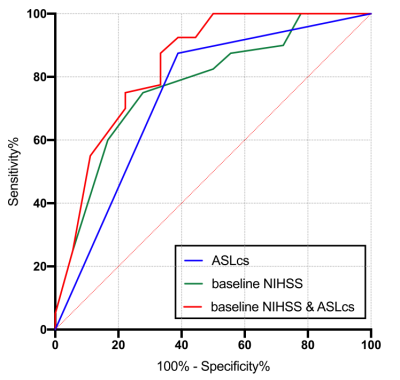
RESULTS A total of 58 patients(mean age, 64.0 ± 12.0 years [standard deviation]; 42 men) were included.Patients’ characteristics are summarized in Figure 1. Patients with ASL collaterals represented higher rate of good outcome (follow-up mRS score of 0-2)(83.3% vs. 31.25%, P< 0.001) and lower follow-up mRS score(P< 0.001), when compared to that without ASL collateral circulation( Figure 2). There were significant differences for percent changes of mRS score(P<0.05) and NIHSS score (P<0.05) between groups(Figure 3). In multivariable logistic regression analysis, the presence of ASL collaterals could predict good outcome (OR 1.54, 95% CI 1.1 - 2.16, p=0.012), even after controlling for baseline NIHSS score(Figure 4). ROC curve analysis revealed that the presence of ASL collaterals had significant predictive value (AUC, 0.74; 95% CI: 0.59 - 0.89; P = 0.003) for a favorable 90-day mRS score(Figure 5).
DISCUSSION Collateral circulation is of paramount importance to acute ischemic stroke. In this study, we targeted at collaterals using ASL, a functional neuroimaging technique without injecting contrast. Our data demonstrated that patients with ASL collaterals tended to have lower baseline NIHSS score, follow-up mRS score, and higher rates of good clinical outcome. Regardless of the presence or absence ASL collaterals, changing trends of mRS score and NIHSS score were downward, and that of BI score was growing as time went on. This changing trends, when characterized using percent change of scores, had significant differences in mRS and NIHSS scores between groups. Furthermore, after adjusting for the potential confounder, which is baseline NIHISS score in this study, patients with ASL collaterals were about 1.5-fold more likely to come to a good clinical outcome. ASL collateral circulation was demonstrated to have significant predictive value for good clinical outcome after stroke in our study. Taken together, our results suggest that ASL-based collateral circulation is significantly associated with and is a predictive factor of good clinical outcome after acute ischemic stroke. In recent studies, collaterals defined as ATA in ASL images were compared with DSA in patients with Moyamoya disease, results revealing that agreements between ASL and DSA was substantial6,7. This agreements for collaterals detecting were also confirmed in patients with internal carotid artery or intracranial arterial steno-occlusive disease, or with ischemic stroke8-11. Besides, the presence of collateral circulation on ASL has been associated with progress and prognosis of disease in recent research. ATA in ASL images has been proved to be associated with recent ischemic symptoms in patients with carotid stenosis12. The presence of collaterals blood vessels, defined as ATA in ASL images, was observed to be associated with admission NIHSS score and lower median mRS scores at discharge3. Our study expanded on this work, and demonstrated collateral circulation detected by ASL was associated with good clinical outcome and better improvement measured by percent change of NIHSS and mRS scores 90 days after AIS.
CONCLUSION Our results demonstrated that patients with ASL collateral circulation had a propensity for better clinical outcome after AIS, and ASL collaterals could predict good clinical outcome even when controlled for baseline NIHISS score. These findings indicate that the presence of ASL collaterals is a significant predictor of good clinical outcome after acute ischemic stroke.
Acknowledgements
My deepest gratitude goes first and foremost to Professor Xie Chunming, my tutor, for his constant encouragement and guidance. Then, I pleased to acknowledge team colleagues for their cooperation, comments, and wise advice. Finally, in particular, I would like to express my gratitude to subjects involved in our study.References
1.Campbell BCV, Khatri P. Stroke. Lancet. 2020;396(10244):129-142. doi:10.1016/S0140-6736(20)31179-X
2.Boulouis G, Lauer A, Siddiqui AK, et al. Clinical Imaging Factors Associated With Infarct Progression in Patients With Ischemic Stroke During Transfer for Mechanical Thrombectomy. JAMA Neurol. 2017;74(11):1361-1367. doi:10.1001/jamaneurol.2017.2149
3.de Havenon A, Haynor DR, Tirschwell DL, et al. Association of Collateral Blood Vessels Detected by Arterial Spin Labeling Magnetic Resonance Imaging With Neurological Outcome After Ischemic Stroke. JAMA Neurol. 2017;74(4):453-458. doi:10.1001/jamaneurol.2016.4491
4.Lin L, Yang J, Chen C, et al. Association of Collateral Status and Ischemic Core Growth in Patients With Acute Ischemic Stroke. Neurology. 2021;96(2):e161-e170. doi:10.1212/WNL.0000000000011258
5.Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME, Steinberg GK. Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with moyamoya disease. Stroke. 2011;42(9):2485-2491. doi:10.1161/STROKEAHA.111.616466
6.Hwang I, Cho WS, Yoo RE, et al. Revascularization Evaluation in Adult-Onset Moyamoya Disease after Bypass Surgery: Superselective Arterial Spin Labeling Perfusion MRI Compared with Digital Subtraction Angiography. Radiology. 2020;297(3):630-637. doi:10.1148/radiol.2020201448
7.Lee S, Yun TJ, Yoo RE, et al. Monitoring Cerebral Perfusion Changes after Revascularization in Patients with Moyamoya Disease by Using Arterial Spin-labeling MR Imaging. Radiology. 2018;288(2):565-572. doi:10.1148/radiol.2018170509
8.Wu EZ, Liu X, Dornbos D 3rd, et al. Comparison of 3D Multi-inversion Time Arterial Spin Labeling and Digital Subtraction Angiography in the Evaluation of Cerebral Collateral Circulation. CNS Neurosci Ther. 2016;22(12):1009-1011. doi:10.1111/cns.12603
9.Chng SM, Petersen ET, Zimine I, Sitoh YY, Lim CC, Golay X. Territorial arterial spin labeling in the assessment of collateral circulation: comparison with digital subtraction angiography. Stroke. 2008;39(12):3248-3254. doi:10.1161/STROKEAHA.108.520593
10.Wu B, Wang X, Guo J, et al. Collateral circulation imaging: MR perfusion territory arterial spin-labeling at 3T. AJNR Am J Neuroradiol. 2008;29(10):1855-1860. doi:10.3174/ajnr.A1259
11.Iryo Y, Hirai T, Nakamura M, et al. Collateral circulation via the circle of Willis in patients with carotid artery steno-occlusive disease: evaluation on 3-T 4D MRA using arterial spin labelling. Clin Radiol. 2015;70(9):960-965. doi:10.1016/j.crad.2015.05.002
12.Di Napoli A, Cheng SF, Gregson J, et al. Arterial Spin Labeling MRI in Carotid Stenosis: Arterial Transit Artifacts May Predict Symptoms. Radiology. 2020;297(3):652-660. doi:10.1148/radiol.2020200225
Figures