4573
Detection of crossed cerebellar diaschisis in subacute ischemic stroke using 3D PCASL with two post-labeling delay time method1Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China, 2MR Research China, GE Healthcare, Beijing, China
Synopsis
This study investigated the feasibility of 3D PCASL to detect crossed cerebellar diaschisis (CCD) in patients with unilateral supratentorial subacute stroke using two PLD method and correlated the ischemic perfusion with CCD to identify the relevant imaging factors of CCD development. 3D PCASL can detect CCD in patients of supratentorial subacute stroke. Patients of supratentorial subacute stroke experience late-arriving flow while CCD+ patients suffer late arriving flow in the affected contralateral cerebellum. CCD+ patients may have a propensity towards more hemodynamic compromise and compensatory collateral flow in the cerebellum.
Introduction
Crossed cerebellar diaschisis (CCD) is a common radiological phenomenon manifested as reduced blood flow and glucose metabolism in the cerebellar hemisphere contralateral to a supratentorial cerebral lesion, while whether the extent of supratentorial cerebral ischemia influences CCD was still inconsistent1.This study aimed to evaluate the ability of 3D FSE pseudo-continuous ASL perfusion imaging (PCASL) to detect CCD in patients with unilateral supratentorial subacute stroke using two post-labeling delay time (PLD) method, correlate the ischemic perfusion with CCD and to identify the relevant imaging factors of CCD development.
Methods
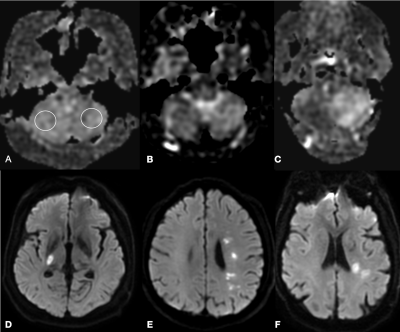
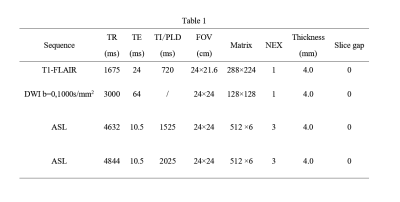
Thirty-three patients with subacute unilateral supratentorial ischemic stroke were retrospectively recruited in the study. All MRI scans were accomplished on a 3.0T MR scanner (Discovery 750, GE Healthcare, Milwaukee, WI) with an 8-channel phase-array head coil. The imaging parameters in axial plane are listed in Table 1. Acquisition time of ASL for each PLD was 3.5 minutes. Two radiologists evaluated the cerebellar CBF maps of both PLD from inferior to superior slices according to a three-grade method 2, shown in Figure 1. A Grade of 2 or 3 was considered a positive CCD. The CBF of the infarct lesion and its contralateral side,the affected cerebellar hemisphere and ipsilateral normal side were measured at both PLD. The asymmetric index (AI) of both PLD between the contralateral and ipsilateral cerebellar hemisphere to the infarction was calculated as:AI=[(CBF ipsilateral cerebellum-CBF contralateral cerebellum)/ CBF ipsilateral cerebellum] ×100%.
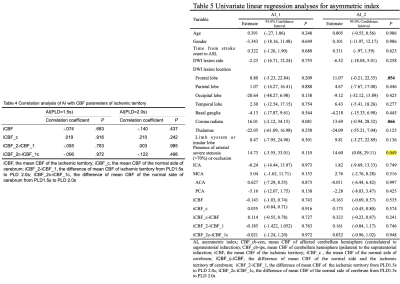
CBF measurements were compared between two PLDs, ischemic territory and normal side, CCD+ and CCD- patients respectively. Thereafter, correlation analysis and regression analysis were performed for AI and all clinical and MR imaging factors to identify factors independently associated with AI.
Results
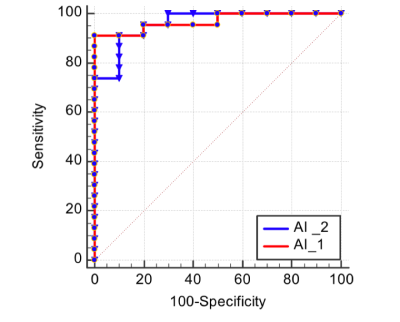
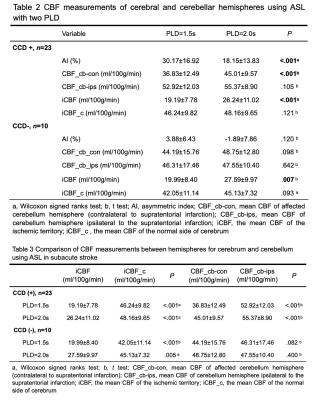
Representative patients of CCD+ group were shown in Figure 1.ROC analysis demonstrated that the AI at both PLD had equivalent diagnostic performance in detection of CCD in patients with subacute stroke (Figure 2). Although the AUC between two AI was not significantly different, AI at PLD 1.5s was higher than that of PLD 2.0s in all patients and the CCD+ group ( P<.001, Table 2).
In the CCD+ group and CCD- group, the CBF of the ischemic territory both increased significantly from 1.5s to 2.0s (P=.001 or .007, Table 2) and it’s significantly lower than the normal side at both PLD (P< 0.001 or =.005,Table 3). While mean CBF in the normal side were with no significant change from PLD 1.5s to 2.0 s in both groups (P=.601). The mean CBF increased similarly from PLD 1.5 to 2.0 s on the ischemic territory between CCD+ group and CCD- group (P=.800).
In the CCD+ group, mean CBF of the affected contralateral cerebellar hemisphere increased significantly from PLD 1.5s to 2.0s (P<.001, Table2), while CBF of the ipsilateral cerebellar hemisphere showed no significant difference between PLD 1.5s and 2.0s. The mean CBF of the affected hemisphere was lower than ipsilateral unaffected hemisphere at both PLDs (P<.001 for both PLD, Table 3).
In the CCD- group, mean CBF of the contralateral cerebellar hemisphere (CBF_cb-con) and the ipsilateral cerebellar hemisphere (CBF_cb-ips) showed no significant differences between both PLDs (P=0.098 and 0.042). The mean CBF of the contralateral cerebellum hemisphere showed similar with that of ipsilateral hemisphere at both PLDs (P=.082 and .400).
Pearson or Spearman correlation analysis revealed that there was no significant correlation between AI and CBF measurements (iCBF, iCBF_c and their difference between two PLD, Table 4). Linear regression analysis (P=0.049, Table 5) and multiple regression analyses proved that presence of arterial severe stenosis or occlusion was the only variable significantly associated with AI of PLD 2.0s in patients with subacute ischemic stroke (estimates, 15.44; 95% CI, [.396, 30.484]; P= .045).
Discussion
3D PCASL with multiple PLDs has potential advantages over single delay PCASL scans, including improved accuracy of CBF quantification, visualization, and quantification of collateral flow in patients of stroke and patients with intracranial artery stenosis3-5. The present study utilizing two PLDs illustrates that the 3D PCASL sequence is a useful tool to detect CCD in patients of subacute stroke (69.7%) with equivalent diagnostic performance at PLD 1.5s and 2.0s. We indicate that patients of supratentorial subacute stroke experience late-arriving flow (antegrade delayed flow and collateral retrograde flow) in the ischemic cerebral territory, which is consistent with previous results4. Although CCD+ patients had similar supratentorial hypoperfusion with CCD- patients, our data implies that CCD+ patients suffer slow antegrade blood flow and late-arriving antegrade flow and collateral retrograde flow in the affected contralateral cerebellar hemisphere, which, to some extent, validates the opinion that CCD+ shows a propensity towards more hemodynamic compromise and compensatory collateral flow6. Regression analysis reveals that the presence of CCD in subacute ischemic stroke may imply a greater probability of arterial severe stenosis or occlusion.Conclusion
PCASL can effectively and noninvasively detect CCD in patients of supratentorial subacute stroke. Supratentorial subacute stroke experience late-arriving flow while CCD+ patients suffer late arriving flow in the affected contralateral cerebellum. CCD+ patients with a greater probability of arterial severe stenosis or occlusion, have a propensity towards more hemodynamic compromise and compensatory collateral flow in the cerebellum.Acknowledgements
No acknowledgement found.References
1. Zhang M, Cao Y, Wu F, et al. Characteristics of cerebral perfusion and diffusion associated with crossed cerebellar diaschisis after acute ischemic stroke. Jpn J Radiol 2020 Feb;38(2).
2. Kang KM, Sohn C, Choi SH, et al. Detection of crossed cerebellar diaschisis in hyperacute ischemic stroke using arterial spin-labeled MR imaging. Plos One 2017;12(3):e173971.
3. Lou X, Ma X, Liebeskind DS, et al. Collateral perfusion using arterial spin labeling in symptomatic versus asymptomatic middle cerebral artery stenosis. J Cereb Blood Flow Metab 2019;39(1):108-117.
4. Lyu J, Ma N, Liebeskind DS, et al. Arterial Spin Labeling Magnetic Resonance Imaging Estimation of Antegrade and Collateral Flow in Unilateral Middle Cerebral Artery Stenosis. Stroke 2016;47(2):428-433.
5. Lou X, Yu S, Scalzo F, et al. Multi-delay ASL can identify leptomeningeal collateral perfusion in endovascular therapy of ischemic stroke. Oncotarget 2017;8(2):2437-2443.
6. von Bieberstein L, van Niftrik C, Sebok M, et al. Crossed Cerebellar Diaschisis Indicates Hemodynamic Compromise in Ischemic Stroke Patients. Transl Stroke Res 2021;12(1):39-48.
Figures