4570
The Clinical value of Left ventricle and Septum for Right ventricular function in Patients with Left Ventricle Acute Myocardial Infarction
Yanan Zhao1, Tao Li1, Jianing Cui1, Xueqian Liu2, and Xiuzheng Yue3
1Department of Radiology, Chinese People’s Liberation Army General Hospital, Beijing, China, 2Qinhuangdao Workers' Hospital, Qinhuangdao, China, 3Philips Healthcare, Beijing, China
1Department of Radiology, Chinese People’s Liberation Army General Hospital, Beijing, China, 2Qinhuangdao Workers' Hospital, Qinhuangdao, China, 3Philips Healthcare, Beijing, China
Synopsis
The reduced right ventricular ejection fraction (RVEF) has prognostic value for predicting cardiovascular mortality in patients with left ventricular acute myocardial infarction (LVAMI). Previous studies have shown that interaction between left ventricular (LV) and right ventricular (RV). This study used CMR to further explore what factors affect the RVEF. The results shown that the incidence of reduced RVEF was 40% in LVAMI patients and the occurrence of reduced RVEF was associated with LVEF, LV end-systolic volume index and RV end-systolic volume index.
Introduction
Recent studies[1, 2] shown that reduced right ventricular ejection fraction (RVEF) provides prognostic value predicting cardiovascular mortality in patients with left ventricular acute myocardial infarction (LVAMI). However, there was few studies on predictors for the occurrence of reduced RVEF in patients with LVAMI. In this study, we use CMR to explore whether the function of the RV is affected by the function of the LV and the interevent ridular septum (IVS).Methods:
From January 2017 to December 2020, Consecutive identified LVAMI (according to the ESC/ACC committee criteria[3]) patients underwent Cardiac magnetic resonance (CMR) 1-7 days after successfully percutaneous coronary intervention (Figure 1). The imaging protocol included cine imaging and late gadolinium enhancement (LGE). The short-axis LGE images was used for visualizing scar of left ventricular (LV) and right ventricular (RV), and to calculate infarction size of LV by using the full-width-at-half maximum method[4]. Microvascular obstruction (MVO) of LV was identified on the LGE images as a hypointense core within scar (hyper-enhanced myocardium)[5]. The RV and LV function were measured by CMR-FT from cine images. The RVEF = 50% (according to CMR-FT from cine images) was used as the cutoff value to divide the study population with LVAMI into reduced RVEF or non- Reduced RVEF. On the 16-segment model, the IVS (2、3、8、9 and 14) are treated as a whole (Figure 2). The RV and LV function in patients with and without reduced RVEF were compared by using independent-samples t-test. Univariate and multivariable conditional binary logistic regression analyses were performed to find factors associated with reduced RVEF.Results
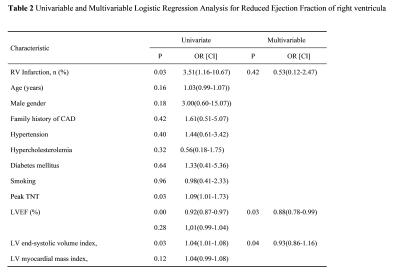
87 patients with LVAMI (55±11 years of age; 11% women, mean LVEF 46 ± 9%) underwent RV function assessment using CMR-FT. Of the 87 patients, 35 (40%) had reduced RVEF. Baseline characteristics of patients with reduced RVEF and non- Reduced RVEF are presented in. Within the Reduced RVEF group, the number of patients with RV infarction was high (11/35;31% vs 6/52;12%, P=0.03). As shown in Table 1, the patients with reduced RVEF presented with significantly lower LVEF, LV circumferential peak strain (P<0.01, P=0.02) and higher LV end-systolic volume index (P=0.03) compared with the non- Reduced RVEF group. Compared to with non-reduced RVEF, IVS Average wall thickening rate was also significantly decreased in LVAMI patients with reduced RVEF (P = 0.01). Within the Reduced RVEF group, patients demonstrated greater LV infarct size and IVS infarct size. In a multivariable stepwise forward logistic regression analysis, the presence of reduced RVEF was independently associated with LVEF (odds ratio, 0.88; 95% CI, 0.78-0.99 [P=0.03]), LV end-systolic volume index (odds ratio, 0.93; 95% CI, 0.86-1.16 [P=0.04]) and RV end-systolic volume index (odds ratio, 1.20; 95% CI, 1.10-1.32 [P<0.01]) (Table 2).Discussion:
In clinical work, we often pay more attention on the LV function of patients with LVAMI[6, 7] rather than RV function. Our study showed that the incidence of decreased RVEF was 40%, a large proportion of patients with LVAMI. And prior studies showed that RV function predicts prognosis in AMI[8]. Our experiments have further found that lower LVEF and IVS average wall thickening rate increase the incidence of decreased RVEF. This is consistent with previous studies that there is an interaction between the LV and RV[9].Conclusion:
Reduced RVEF was detected in 40% LVAMI patients. Occurrence of reduced RVEF was associated with LVEF, LV end-systolic volume index and RV end-systolic volume index.Acknowledgements
No acknowledgement found.References
[1] L. Houard, M.B. Benaets, C. de Meester de Ravenstein, et al., Additional Prognostic Value of 2D Right Ventricular Speckle-Tracking Strain for Prediction of Survival in Heart Failure and Reduced Ejection Fraction: A Comparative Study With Cardiac Magnetic Resonance, JACC. Cardiovascular imaging 12 (2019) 2373-2385. [2] B. Ibanez, A.H. Aletras, A.E. Arai, et al., Cardiac MRI Endpoints in Myocardial Infarction Experimental and Clinical Trials: JACC Scientific Expert Panel, Journal of the American College of Cardiology 74 (2019) 238-256. [3] K. Thygesen, J.S. Alpert, A.S. Jaffe, et al., Third universal definition of myocardial infarction, European heart journal 33 (2012) 2551-2567. [4] A.S. Flett, J. Hasleton, C. Cook, et al., Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance, JACC. Cardiovascular imaging 4 (2011) 150-156. [5] T. Podlesnikar, G. Pizarro, R. Fernández-Jiménez, et al., Left ventricular functional recovery of infarcted and remote myocardium after ST-segment elevation myocardial infarction (METOCARD-CNIC randomized clinical trial substudy), Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance 22 (2020) 44. [6] T. Stiermaier, S.J. Backhaus, T. Lange, et al., Cardiac Magnetic Resonance Left Ventricular Mechanical Uniformity Alterations for Risk Assessment After Acute Myocardial Infarction, Journal of the American Heart Association 8 (2019) e011576. [7] R.P. Amier, R.Y.G. Tijssen, P.F.A. Teunissen, et al., Predictors of Intramyocardial Hemorrhage After Reperfused ST-Segment Elevation Myocardial Infarction, Journal of the American Heart Association 6 (2017). [8] M. Grothoff, C. Elpert, J. Hoffmann, et al., Right ventricular injury in ST-elevation myocardial infarction: risk stratification by visualization of wall motion, edema, and delayed-enhancement cardiac magnetic resonance, Circulation. Cardiovascular imaging 5 (2012) 60-68. [9] F. Haddad, R. Doyle, D.J. Murphy, et al., Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure, Circulation 117 (2008) 1717-1731.Figures
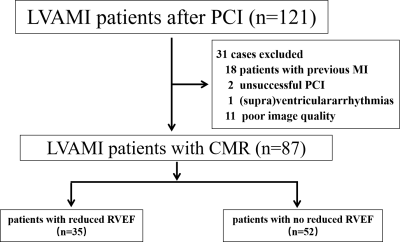
Figure 1 the flowchart of patient
enrollment. CMR, cardiac magnetic resonance; LVAMI, left ventricular acute
myocardial infarction
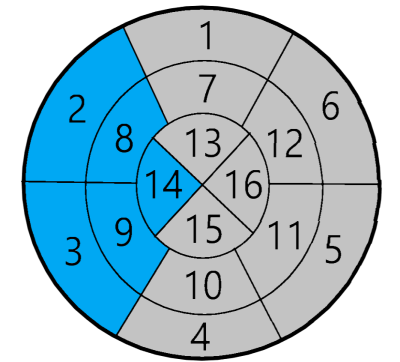
Figure 2 Schematic diagram of the interevent ridular
septum, the interevent ridular septum are the segments 2,3,8,9 and 14
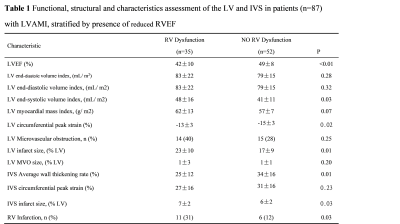
LV, left ventricular; RV, right ventricular; MVO,
Microvascular obstruction; IVS,interevent ridular septum.
LV, left ventricular; RV, right ventricular; MVO, Microvascular obstruction; IVS,interevent ridular septum.
DOI: https://doi.org/10.58530/2022/4570